
 Download the whole Issue
Download the whole Issue
LEADING ARTICLE
ORIGINAL RESEARCH
REVIEWS
ORGANIZATION OF HEALTHCARE
MEDICIN’S HISTORY
CLINICAL CASE
___
 PILOT PROJECT OF INTERREGIONAL INTERACTION OF MEDICAL SUPPLY ON THE BASIS OF THE MEDICAL UNIT OF THE INTERNAL AFFAIRS OF RUSSIA IN THE REPUBLIC OF TATARSTAN
PILOT PROJECT OF INTERREGIONAL INTERACTION OF MEDICAL SUPPLY ON THE BASIS OF THE MEDICAL UNIT OF THE INTERNAL AFFAIRS OF RUSSIA IN THE REPUBLIC OF TATARSTAN
UDC 614.21:351.74(470.41):616-07
DOI: 10.20969/VSKM.2017.10(4).7-11
KHISAMIEV RUSTEM SH., major of internal service, Head of the Medical Unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan, Russia, 420101, Kazan, Lobachevsky str., 13, e-mail: msch_16@mvd.gov.ru
GINJATULLINA LJASAN R., lieutenant colonel of internal service, Deputy chief of the Unit, physician of the Medical Unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan, Russia, 420101, Kazan, Lobachevsky str., 13
AMIROV NAIL B., D. Med. Sci., academician of Russian Academy of Natural Science, professor of the Department of general medical practice of Kazan State Medical University, Russia, 420012, Butlerov str., 49, e-mail: namirov@mail.ru
Abstract. Significant part of the complex of rendering medical service in the system of departmental health of the Ministry of Internal Affairs belongs to diagnostic process. It can be characterized by staff referral to the third-party medical and preventive institutions of the Republic of Tatarstan in order to perform certain diagnostic procedures. Aim. The pilot project on interregional interaction of medical supply on the basis of the Medical unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan has been created. Material and methods. Analysis of diagnostic service has been performed in the Clinical Hospital of the Medical Unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan, as well as in the neighboring regions. Results and discussion. Analysis of the diagnostic service has shown an increase in the annual load for each unit of diagnostic and laboratory equipment and, consequently, for the doctors conducting the examinations. Available areas do not allow the introduction of additional examination methods or upgrading the diagnostic equipment of the medical unit. In order to unify and strengthen the diagnostic capabilities of the outpatient clinic and hospital it was decided by the leaders of the Department of Material, technical and medical supply of the Ministry of Internal Affairs of Russia, to establish Interregional consultative diagnostic center at the Clinical Hospital of the Medical Unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan in the framework of interregional interaction for medical service provision to the employees of the Ministry of Internal Affairs of Russia in the Volga region. Conclusion. The introduction of modern high-tech diagnostic methods based on the concentration and intensive use of the newest means will allow more precise patient examination, improve the quality and accessibility of medical care and health promotion for employees of the Ministry of Internal Affairs. Consequently, it will lead to successful accomplishment of the assigned service tasks.
Key words: medical service, Internal Affairs Bodies, interregional cooperation, diagnostic center.
For reference: Khisamiev RSh, Ginjatullina LR, Amirov NB. Pilot project of interregional interaction of medical supply on the basis of the Medical unit of the Ministry of internal affairs of Russia in the Republic of Tatarstan. The Bulletin of Contemporary Clinical Medicine. 2017; 10 (4): 7—11. DOI: 10.20969/ VSKM.2017.10(4).7-11.
 SELECTED EPIDEMIOLOGICAL AND MICROBIOLOGICAL ASPECTS OF MORBIDITY OF COMMUNITY-ACQUIRED PNEUMONIA
SELECTED EPIDEMIOLOGICAL AND MICROBIOLOGICAL ASPECTS OF MORBIDITY OF COMMUNITY-ACQUIRED PNEUMONIA
UDC 616.24-002-036.22-057.36(470.53)
DOI: 10.20969/ VSKM.2017.10(4).12-15
BABUSHKIN SERGEY A., Head of the Center for State Sanitary and Epidemiological Surveillance of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Perm region, Russia, 614000, Perm, Permskaya str., 128, e-mail: medmicrobiolog@gmail.com
IVENSKIKH VIKTOR I., Head of the Department of epidemiology of the Center for State Sanitary and Epidemiological Surveillance of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Perm region, Russia, 614000, Perm, Permskaya str., 128, e-mail: medmicrobiolog@gmail.com
GODOVALOV ANATOLIY P., ORCID ID: orcid.org/0000-0002-5112-2003, C. Med. Sci., bacteriologist of the Center for State Sanitary and Epidemiological Surveillance of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Perm region, Russia, 614000, Perm, Permskaya str., 128, e-mail: AGodovalov@gmail.com
OZHGIBESOV GEORGY P., Head of the bacteriological laboratory of the Center for State Sanitary and Epidemiological Surveillance of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Perm region, Russia, 614000, Perm, Permskaya str., 128, e-mail: medmicrobiolog@gmail.com
SHUBINA NADEZHDA V., epidemiologist of the Center for State Sanitary and Epidemiological Surveillance of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Perm region, Russia, 614000, Perm, Permskaya str., 128, e-mail: medmicrobiolog@gmail.com
Abstract. Aim. The features of the long-term morbidity and sputum microflora composition in community-acquired pneumonia in employees of the Ministry of Internal Affairs of Russia in the Perm region have been studied. Material and methods. The manifestations of the epidemic process of community-acquired pneumonia in employees of the Ministry of Internal Affairs of Russia in the Perm region have been analysed. Microbiological examination of 560 sputum specimens has been conducted in order to determine the etiology of pneumonia. Statistical processing of the data has been carried out using Student’s t-test and Spearman correlation coefficient. Results and discussion. In the course of conducted studies it was shown that the incidence of community-acquired pneumonia in employees of the Ministry of Internal Affairs of Russia in the Perm region has a number of peculiarities. The changes in the spectrum of microorganisms causing the disease have been revealed. So that, in the overwhelming majority of cases pneumonia was caused by Streptococcus spp. with a relatively small proportion of S. pneumoniae. The essential role of yeastlike fungi Candida spp. and Staphylococcus spp. in development of the disease was shown. In more than half of the cases microbial associations represented mainly by Gram-positive cocci have been identified. In turn, the increase in morbidity correlates with the increase in shedding of enterococci and enterobacteria. Conclusion. In general, there is a tendency for an increase in the incidence of community-acquired pneumonia. It might be related to the changes in etiologic structure of the pathogens of the disease, as well as to pathologic symbiosis development by the number of opportunistic pathogenic microorganisms.
Key words: community-acquired pneumonia, pathologic symbiosis, epidemic process, microbial associations.
For reference: Babushkin SА, Ivenskikh VI, Godovalov AP, Ozhgibesov GP, Shubina NV. Selected epidemiological and microbiological aspects of morbidity of community-acquired pneumonia. The Bulletin of Contemporary Clinical Medicine. 2017; 10 (4): 12—15. DOI: 10.20969/ VSKM.2017.10(4).12-15.
Refereneces
1. Chuchalin AG, Sinopal’nikov AI, Kozlov RS, Tjurin IE, Rachina SA. Vnebol’nichnaja pnevmonija u vzroslyh: prakticheskie rekomendacii po diagnostike, lecheniju i profilaktike [Community-acquired pneumonia and adults: practical recommendations for diagnosis, treatment and prevention]. Klinicheskaja mikrobiologija i antimikrobnaja himioterapija [Clinical microbiology and antimicrobial chemotherapy]. 2006; 8 (1): 54-86.
2. Babushkin SA, Ivenskih VI, Mamaev AV, Ozhgibesov GP, Nikulina EA, Shubina NV, Godovalov AP. Jepidemiologicheskie i mikrobiologicheskie aspekty zabolevaemosti ostrymi faringitami i tonzillitami sotrudnikov MVD Rossii po Permskomu kraju [Epidemiological and microbiological aspects of the incidence of acute pharyngitis and tonsillitis of employees of the Ministry of Internal Affairs of Russia for the Perm region]. Vestnik sovremennoj klinicheskoj mediciny [Herald of modern clinical medicine]. 2016; 9 (6): 27-33.
3. Shubin IV. Aktual’nost’ vakcinoprofilaktiki pnevmokokkovoj infekcii v organizovannyh kollektivah voennosluzhashhih [The urgency of vaccine prophylaxis for pneumococcal infection in organized groups of servicemen]. Vestnik sovremennoj klinicheskoj mediciny [The Bulletin of Contemporary Clinical Medicine]. 2017; 10 (1): 36-42.
4. Godovalov AP, Bykova LP. Osobennosti Candida sp. iz mikrobnyh associacij pri vospalitel’nyh zabolevanijah dyhatel’nyh putej [Features of Candida sp. from microbial associations in inflammatory diseases of the respiratory tract]. Uspehi medicinskoj mikologii [Advances in medical mycology]. 2013; 11: 84-87.
5. Callagova OT, Gatagonova TM, Bolieva LZ. Struktura bakterial’nyh vozbuditelej vnebol’nichnoj pnevmonii u gospitalizirovannyh bol’nyh v RSO-Alanija [Structure of bacterial pathogens of community-acquired pneumonia in hospitalized patients in the Republic of North Ossetia-Alania]. Sovremennye problemy nauki i obrazovanija [Modern problems of science and education]. 2014; 6: 45-48.
6. Beljakov VD, Semenenko TA, Shraga MH. Vvedenie v jepidemiologiju infekcionnyh i neinfekcionnyh zabolevanij cheloveka [Introduction to the epidemiology of infectious and non-infectious human diseases]. Moskva: Medicina [Moscow: Medicine]. 2001: 264 p.
7. Sepetliev DM. Statisticheskie metody v nauchnyh medicinskih issledovanijah [Statistical methods in scientific medical research]. Moskva: Medicina [Moscow: Medicine]. 1968: 298 p.
8. Godovalov AP, Bykova LP, Ozhgibesov GP. Znachenie gribov roda Candida pri vospalitel’nyh zabolevanijah dyhatel’nyh putej [The importance of fungi of the genus Candida in inflammatory diseases of the respiratory tract]. Sibirskij medicinskij zhurnal (Irkutsk) [Siberian Medical Journal (Irkutsk)]. 2008; 82 (7): 10-12.
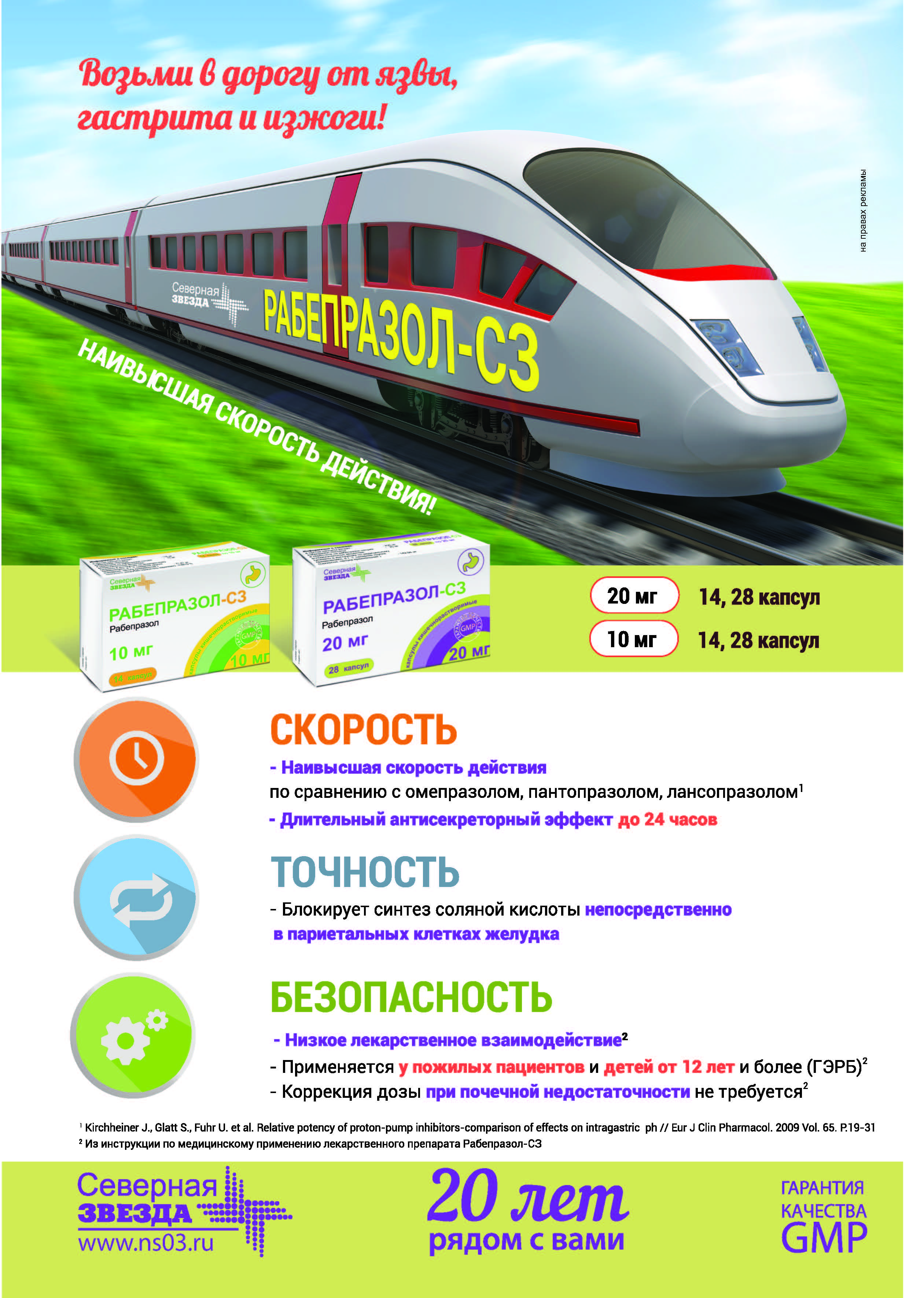
 COMPARATIVE ANALYSIS OF EFFECTIVENESS OF RABEPRAZOLE AND OMEPRAZOLE IN GASTROESOPHAGEAL REFLUX DISEASE
COMPARATIVE ANALYSIS OF EFFECTIVENESS OF RABEPRAZOLE AND OMEPRAZOLE IN GASTROESOPHAGEAL REFLUX DISEASE
UDC [616.33-008.17-031:611.329]-085.243.4
DOI: 10.20969/ VSKM.2017.10(4).16-22
GIMALETDINOVA IRINA A., gastroenterologist of Clinical hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan, Russia, 420059, Kazan, Orenburg tract str., 132, tel. +7-903-313-12-27, e-mail: iren-kaz@mail.ru
ABSALYAMOVA LEJLE R., Head of the Department of gastroenterology of Clinical hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan, Russia, 420059, Kazan, Orenburg tract str., 132, tel.+7-965-608-72-73
AMIROV NAIL B., D. Med. Sci., professor of the Department of general medical practice of Kazan State Medical University, Russia, 420012, Kazan, Butlerov str., 49, e-mail: namirov@mail.ru
Abstract. Gastroesofageal reflux disease is a condition that occurs when stomach content reflux causes patient symptoms and/or complications. Gastroesophageal reflux became an independent disease at the end of the 20 century due to its high incidence and permanent tendency to growth. The first choice in the treatment of the disease is proton pump inhibitors. Aim. Comparative analysis of effectiveness of gastroesophageal disease treatment (uncomplicated and erosive) with proton pump inhibitors: omeprazole administered in the dose of 40 mg/day 30 minutes before breakfast and rabeprazole-C3 in enteric soluble capsules in a dose of 20 mg/day 30 minutes before breakfast (administration regardless of the meal is possible) in combination with antacids, prokinetics in standard doses in terms of symptom reduction and healing of reflux-esophagitis. Material and methods. The results of the clinical study of two groups of patients observed, 20 people each, aged 25 to 65 years, are presented. The mean patient age was 45 years. Duration of the study was 4 weeks (28 days). Results and discussion. The obtained data testifies the effectiveness of rabeprazole-C3 in treatment of gastroesophageal reflux disease. It provides a fast and steady symptom relief, which improves adherence and compliance to therapy in 100% of patients. Conclusion. 20 mg/day of Rabaprazole-C3 in gastroesophageal reflux disease helps to reduce the severity of heartburn and dyspepsia faster compared to omeprazole in the dose of 40 mg/day, especially in case of strictly following recommendations on changing lifestyle and habits, as well as it promotes faster healing of erosion and regeneration of normal esophageal mucosa. Good tolerance to a four-week course of treatment with Rabeprazole-C3 was seen.
Key words: rabeprazole, cytochrome CYP450, compliance, survey GerdG.
For reference: Gimaletdinova IA, Absalyamova LR, Amirov NB. Comparative analysis of effectiveness of rabeprazole and omeprazole in gastroesophageal reflux disease. The Bulletin of Contemporary Clinical Medicine.2017; 10 (4): 16—22. DOI: 10.20969/ VSKM.2017.10(4).16-22.
Refereneces
1. Vakil N, van Zanzen SV, Kabrilas Pet al. Te Monreal Definition and Classification of Gastroesophageal Reflux Disease: A Global Evidence-Based Consensus. Am j Gastroenterol. 2006; 101: 1900-1920.
2. Lazebnik LB, Masharova AA, Bordin DS et al. Rezul’taty Mnogocentrovogo issledovanija «Jepidemiologija Gastrojezofageal’noj REfljuksnoj bolezni v Rossii» (MJeGRE) [Results of the Multicentre Study «Epidemiology of Gastroesophageal Reflux Disease in Russia» (MEGRE)]. Terapevticheskij arhiv [Therapeutic archive].
2011; 1: 45–50.
3. Dent J, El-Serag HB, Wallander MA et al. Epidemiology of gastro-esophageal reflux disease: A systematic reveiew. Gut. 2005; 54: 710-717.
4. Ivashkin VT, Truhmanov AS. Sovremennyj podhod k terapii gastrojezofageal’noj refljuksnoj bolezni vo vrachebnoj praktike [Modern approach to the therapy of gastroesophageal reflux disease in medical practice]. Rossijskij medicinskij zhurnal [Russian medical journal]. 2003; 2: 43–48.
5. Ivashkin VT ed. Profilaktika i lechenie hronicheskih zabolevanij verhnih otdelov zheludochno–kishechnogo trakta [Prevention and treatment of chronic diseases of the upper gastrointestinal tract]. Moskva: Medpress — inform [Moscow: Medpress — inform]. 2002; 128 p.
6. Pantoflickova D, Dorta G, Ravik M, Jomod P, Blum A. Acid inhibition on the first day of dosing compassion of four proton pump inhibitors. Aliment Pharmacol Ther. 2003; 17 (12): 1507-1514.
7. Fass R, Fennerty MB, Vakil N. Nonerosive reflux disease — currentconcepts and dilemmas. Am J Gastroenterol. 2001; 96: 303–314.
8. Fass R, Ofman JJ, Gralnek IM et al. Clinical and economicassessment of the omeprazole test in patients with symptoms suggestiveof gastroesophageal reflux
disease. Arch Intern Med. 1999; 159: 2161–2168.
9. Graham DY, Opekun AR, Yamaoka Y et al. Early events in proton pump inhibitor-associated exacerbation of corpus gastritis. Aliment Pharmacol Ther. 2003; 17 (2): 193–200.
10. Galiev ShI, Amirov NB. Duodenogastral’nyj refljuks kak prichina razvitija refljuks-gastrita [Duodenogastric reflux as a cause of the development of reflux gastritis]. Vestnik sovremennoj klinicheskoj mediciny [The Bulletin of Contemporary Clinical Medicine]. 2015; 8 (2): 50-61.
11. Standarty diagnostiki i lechenija kislotozavisimyh i associirovannyh s Helicobacter pylori zabolevanij (chetvertoe Moskovskoe soglashenie)[ Standards
for diagnosis and treatment of acid-dependent and Helicobacter pylori-associated diseases (the Fourth Moscow Agreement)]. Jeksperimental’naja i klinicheskaja gastrojenterologija [Experimental and clinical gastroenterology]. 2010; 5: 113–118: http://www.gastroscan.ru/literature/authors/4230
12. Ingibitory protonnoj pompy: obzor gruppy preparatov [Proton pump inhibitors: a review of the group of drugs]. http://www.pharmacokinetica.ru/news/item/ingibitoryprotonnoj-pompy-obzor-gruppy-preparatov
 СLINICAL AND ANAMNESTIC RISK FACTORS FOR DEVELOPMENT OF GENITAL PROLAPSE IN WOMEN
СLINICAL AND ANAMNESTIC RISK FACTORS FOR DEVELOPMENT OF GENITAL PROLAPSE IN WOMEN
DOI: 10.20969/ VSKM.2017.10(4).23-26
ZIGANSHIN AYDAR M., C. Med. Sci., associate of professor of the Department of obstetrics and gynecology of Bashkir State Medical University, Russia, 450000, Ufa, Lenin str., 3, e-mail: Zigaidar@yandex.ru
NASIBULLIN ILDAR M., C. Med. Sci., associate professor of the Department of topology and operative surgery of Bashkir State Medical University, Russia, 450000, Ufa, Lenin str., 3, e-mail: mvb_bsmu@mail.ru
KUTUSHEV KAMIL G., C. Med. Sci., urologist of Clinic of the Medical Care unit of the Ministry of Internal Affairs of Russia in Republic of Bashkortostan, Russia, 450015, Ufa, K. Marx str., 59
KHALIKOV RUSTEM A., C. Med. Sci., Deputy head of the Hospital, Head of the Department of emergency medicine of the Hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in Republic of Bashkortostan, Russia, 450015, Ufa, K. Marx str., 59
NIGMATULLIN RUSTEM KH., C. Med. Sci., Deputy head of the Medical Care unit of the Ministry of Internal Affairs of Russia in Republic of Bashkortostan, Russia, 450015, Ufa, K. Marx str., 59, e-mail: nigrustem@yandex.ru ;
Abstract. Aim. Medical history and complaints in women with genital prolapse based on clinical and anamnestic data have been studied. Material and methods. Statistical analysis of clinical and anamnestic data in women with genital prolapse admitted for surgical treatment has been carried out on the basis of developed questionnaire. Analysis of medical history and complaints has leaded to genital prolapse risk factor identification. Those are pelvic (disorders of pelvic organs) and common (diseases of different organs and systems). Results and discussion. According to the analysis of clinical and anamnestic data of 176 women, the risk factors that constitute threat in terms of development of genital prolapse are: age (over 50 years), disturbed function of the bladder (84%) and rectum (77%), overweight and obesity (80%), ruptures and trauma of the perineum tissue in vaginal delivery (68%) and heredity (30%), especially the history of descent and prolapse of internal genital organs in mother. Conclusion. Evaluation of clinical and anamnestic data in women over 50 years old, suffering from pelvic organ disorders with the history of perinea rupture in vaginal delivery allows defining risk group for genital prolapse development.
Key words: genital prolapse, descent and abasement of genital organs, medical history, complaints, risk factors.
For reference: Ziganshin AM, Nasibullin IM, Kutushev KG, Halikov RA, Nigmatullin RH. Clinical and anamnestic risk factors for development of genital prolapse in women. The Bulletin of Contemporary Clinical Medicine. 2017; 10 (4): 23—26. DOI: 10.20969/ VSKM.2017.10(4).23-26.
Refereneces
- Apolikhina IA, Dodova YeG, Borodina YeA, Saidova AS, Filippenkova YeV. Disfunkcija tazovogo dna: Sovremennye principy diagnostiki i lechenija [Pelvic Floor Dysfunction: Modern Principles of Diagnostics and Treatment]. Jeffektivnaja farmakoterapija [Effectiv epharmacotherapy]. 2016; 22 (3): 16-23.
- Buyanova SN, Shchukina NA, Zhuravleva AS. Effektivnost ispolzovaniya setchatykh protezov pri oslozhnennykh formakh prolapsa genitalii [The efficiency of the use of mesh prosthesis in complicated forms of genital prolapse]. Rossiiskii vestnik akushera-ginekologa [The Russian Bulletin of the obstetrician-gynecologist]. 2009; 1: 76-81.
- Kulakova VI, Savel’eva GM, Manukhina IB ed. Ginekologiya: natsional’noe rukovodstvo [Obstetrics: national guide.]. Moskva: GEOTAR-Media [Moscow: GEOTAR-Media]; 2009; 1150 p.
- Ziganshin AM, Kulavskii VA. Metod prognozirovaniya riska razvitiya prolapsa tazovykh organov [Method for predicting the risk of pelvic prolapse prolapse]. Tavricheskii medikobiologicheskii vestnik [Taurian medical and biological bulletin.]. 2016; 19 (2): 65-68.
- Ziganshin AM, Fatkullina IB. Effektivnost’ vibromagnitnogo vozdeistviya v lechenii ran promezhnosti u zhenshchin, perenesshikh rody cherez estestvennye rodovye puti [Efficiency of the vibromagnetic effect in the treatment of perineal wounds in women who have transferred labor through natural birth canals]. Lechenie I profilaktika [Treatment and prevention]. 2016; 18 (2): 5-8.
- Ishchenko AI, Aleksandrov LS, Ishchenko AA, Gorbenko OYu, Tarasenko YuN, Khudolei EP, Sulina YaYu, Gavrilova TV. K voprosu o patogeneze tazovoi disfunktsii [On the pathogenesis of pelvic dysfunction]. Voprosy ginekologii, akusherstva ip erinatologii [Questions of gynecology, obstetrics and perinatology]. 2016; 15 (5): 53-58.
- Kulavskii VA, Kulavskii EV, Ziganshin AM. Khirurgicheskaya menopauza u zhenshchin reproduktivnogo vozrasta [Surgical menopause in women of reproductive age]. Akusherstvo ginekologiya I reproduktsiya [Obstetrics gynecology and reproduction]. 2016; 4: 105-113.
- Naftulovich RA, Yashchuk AG, Maslennikov AV, Alakaeva DR. Osobennosti semeinogo anamneza u patsientok s opushcheniem I vypadeniem organov malogo taza [Features of family history in patients with pelvic lowering and prolapse]. Rossiiskii vestnik akushera-ginekologa [The Russian bulletin of the obstetrician-gynecologist]. 2013; 13 (1): 30-36.
- Radzinskiy VE ed. Rukovodstvopo ambulatorno-poliklinicheskoi pomoshchi v akusherstve i ginekologii [A guide to outpatient care in obstetrics and gynecology]. Moskva: GEOTAR-Media [Moscow: GEOTAR-Media]. 2014; 944 p.
- Radzinskii VE. Perineologiya: bolezni zhenskoi promezhnosti v akushersko-ginekologicheskikh, seksologicheskikh, urologicheskikh, proktologicheskikh aspektakh [Perineology: diseases of the female perineum in obstetric-gynecological, sexological, urological, proctological aspects.]. Moskva: MIA [Moscow:MIA]. 2006; 331 p.
- Sukhikh GT, Danilov AYu, Botasheva DA. Rol immunogistokhimicheskikh I geneticheskikh faktorov v utochnenii etiologii I patogeneza prolapsa genitalii u zhenshchin [The role of immunohistochemical and genetic factors in clarifying the etiology and pathogenesis of genital prolapse in women]. Rossiiskii vestnik akushera-ginekologa [The Russian bulletin of the obstetrician-gynecologist. 2012; 12 (2): 47-50.
 SUBJECTIVE MENTAL STATE SELF-ASSESSMENT IN POLICE-COMBATANTS A YEAR AFTER OPERATIONAL SERVICE MISSION IN SPECIAL CONDITIONS
SUBJECTIVE MENTAL STATE SELF-ASSESSMENT IN POLICE-COMBATANTS A YEAR AFTER OPERATIONAL SERVICE MISSION IN SPECIAL CONDITIONS
DOI: 10.20969/ VSKM.2017.10(4).27-32
ICHITOVKINA ELENA G., C. Med. Sci., Head of the Center for psychophysiological diagnostics of Medical Unit of the Ministry of Internal Affairs of Russia in the Kirov region, Russia, 610047, Kirov, Moscovskaya str., 85, e-mail: elena.ichitovckina@yandex.ru
ZLOKAZOVA MARINA V., D. Med. Sci., professor, Head of the Department of psychiatry of Kirov State Medical University, Russia, 610998, Kirov, K. Marx str., 112, e-mail: marinavz@mail.ru SOLOVJOV ANDREY G., D. Med. Sci., professor, Head of the Department of psychiatry and clinical psychology of Northern State Medical University, Russia, 163000, Arkhangelsk, Troitsky ave., 51, e-mail: ASoloviev1@yandex.ru ;
Abstract. Aim. Analysis of subjective mental state self-assessment in police-combatants one year after the operational service mission in special conditions has been performed. Material and methods. Total survey of male combatants who have returned from business trips for operational service and fighting mission in special conditions as a part of composite police detachments for the period 2006—2009 has been carried out in the Center for Psychophysiological Diagnostics at the Medical Unit of the Ministry of Internal Affairs of Russia in the Kirov region. The combatants were divided into 3 groups according to the level of mental health: the 1st group of proficiency — 338 people were healthy combatants without the history of rehabilitation. The 2nd group of proficiency consisted of 311 persons who have demonstrated transient behavioral reactions 6 years prior to the survey according to the data of outpatient cards. During the current survey there was no clinical data on the presence of borderline mental disorders in this group. They have been provided with psychocorrective help by psychologists at the place of their service. The third group of proficiency — 315 people, who had adaptation disorders and post-traumatic stress disorder. They have undergone therapy, medical and psychological rehabilitation for this condition. Results and discussion. It was revealed that the mental state of combatants who have not underwent rehabilitation, is characterized by neurotization and discommunication, reducing the quality of daily routine task performance in places of permanent deployment, which leads to complaints from citizens and undermines public opinion on the police. The weak elements in psychiatric assistance organization to internal affairs bodies’ officers have been identified at the present stage. It was shown, that the disadvantages in psychiatric care organization contribute to hiding mental health problems by internal affairs bodies’ officers and appealing to private practitioners, which leads to the misunderstanding of the real picture of the mental disorder incidence among internal affairs bodies’ employees, reduces the effectiveness of psycho prophylactic work and increases the risk of suicidal and antisocial behavior among internal affairs bodies’ personnel. Conclusion. Establishment of mental health centers in departmental medical units of the Ministry of Internal Affairs of Russia on the basis of existing centers of psychophysiological diagnostics is being proposed. It assumes integration of all departmental specialists in the field of mental health (psychiatrists, psychotherapists, narcologists, clinical and social psychologists of the Ministry of Internal Affairs of Russia); which will imply improving the quality of psychiatric care provision to internal affairs bodies’ employees.
Key words: combatants, mental health, medical and psychological rehabilitation/
For reference: Ichitovkina EG, Zlokazova MV, Soloviev AG. Subjective mental state self-assessment in police-combatants a year after operational service mission in special conditions. The Bulletin of Contemporary Clinical Medicine. 2017; 10 (4): 27—32. DOI: 10.20969/ VSKM.2017.10(4).27-32.
Refereneces
- Agadzhanjan NA, Severin AE. Jekologija i zdorov’e cheloveka: struktura lichnostnyh i obshhestvennyh cennostej [Ecology and human health: the structure of personal and public values]. Zhurnal prikladnoj psihologii [Journal of Applied Psychology]. 2003; 1: 60– 65.
- Ichitovkina EG, Zlokazova MV, Soloviev AG. Efficacy of medical-psychological rehabilitation of combatants [Efficacy of medical-psychological rehabilitation of combatants]. Neuroscience and behavioral physiology [Neuroscience and behavioral physiology]. Springer, New York Consultants Bureau. 2014; 44 (8): 933–938.
- Golokov AV, Shnajder NA, Nikolaeva TJa, Dolinskaja JeA, Solov’eva SF, Golokova EA, Kantimirova EA. Harakteristika i prediktory narushenij sna u sotrudnikov pravoohranitel’nyh organov [Characteristics and predictors of sleep disorders in law enforcement officers]. Vestnik sovremennoj klinicheskoj mediciny [The Bulletin of Contemporary Clinical Medicine]. 2016; 9 (6): 4943.
- Hisamiev RSh, Ginjatullina LR, Amirov NB. Dostizhenija i perspektivy vedomstvennoj medicinskoj sluzhby MVD po respublike Tatarstan [Achievements and prospects of the departmental medical service of the MIA for the Republic of Tatarstan]. Vestnik sovremennoj klinicheskoj mediciny [The Bulletin of Contemporary Clinical Medicine]. 2016; 9 (6): 13-15.
- Korehova MV, Solov’ev AG, Novikova IA. Psihicheskaja dezadaptacija specialistov v jekstremal’nyh uslovijah dejatel’nosti [Psychological disadaptation of specialists in extreme conditions of activity]. Arhangel’sk izdatel’stvo SGMU [Arkhangelsk, publishing house of the Siberian state medical University]. 2014; 139 p.
- Ichitovkina EG, Solov’ev AG, Zlokazova MV, Shutko GV, Har’kova OA. Prognozirovanie vozniknovenija donozologicheskih psihicheskih rasstrojstv u kombatantov [Predicting the emergence of donor psychological disorders in combatants]. Jekologija cheloveka [Human Ecology]. 2016; 10: 47-50.
- Soldatkin VA, Sukiasjan SG, Galkin KJ. Posttravmaticheskoe stressovoe rasstrojstvo: kto na pricele? [Post-traumatic stress disorder: who is on the sight?]. Nauchnometodicheskij jelektronnyj zhurnal «Koncept» [Scientific and Methodical Electronic Journal “Concept”]. 2014; 20: 511–515.
- Prikaz MVD Rossii № 273 «Ob utverzhdenii kompleksnoj Programmy mediko-psihologicheskogo obespechenija sotrudnikov organov vnutrennih del Rossijskoj Federacii i voennosluzhashhih vnutrennih vojsk Ministerstva vnutrennih del Rossijskoj Federacii, vypolnjajushhih zadachi na territorii Severo-Kavkazskogo regiona» [Order of the Ministry of Internal Affairs of Russia # 273 “On the approval of a comprehensive program of medical and psychological support for employees of internal affairs agencies of the Russian Federation and servicemen of internal troops of the Ministry of Internal Affairs of the Russian Federation performing tasks in the North Caucasus region”]. 2004; http://docs.cntd.ru/ document/901905352
- MVD Rossii [Ministry of Internal Affairs of Russia]. Metodicheskie rekomendacii «Vyjavlenie faktorov gruppy riska pri professional’no-psihologicheskom otbore i mediko-psihologicheskom soprovozhdenii lichnogo sostava organov vnutrennih del Rossijskoj Federacii» [Methodological recommendations “Identification of risk factor factors in occupational psychological selection and medical and psychological support for the personnel of the internal affairs bodies of the Russian Federation”]. 2004.
- Ichitovkina EG. Psihicheskoe zdorov’e kombatantov Ministerstva vnutrennih del, v jekstremal’nyh uslovijah operativno-sluzhebnoj dejatel’nosti [Mental health of combatants of the Ministry of Internal Affairs, in extreme conditions of operational and official activities]. Arhangel’sk. 2016; 292 p.
 THE RISK OF SLEEP APNEA SYNDROME DEVELOPMENT AND ITS ADVERSE CARDIOVASCULAR EFFECTS IN WORKING AGE PATIENTS SUFFERING FROM ARTERIAL HYPERTENSION WITH NORMAL BODY WEIGHT OR OBESE
THE RISK OF SLEEP APNEA SYNDROME DEVELOPMENT AND ITS ADVERSE CARDIOVASCULAR EFFECTS IN WORKING AGE PATIENTS SUFFERING FROM ARTERIAL HYPERTENSION WITH NORMAL BODY WEIGHT OR OBESE
UDC 616.24-008.444:616.12-008.331.1
DOI: 10.20969/ VSKM.2017.10(4).32-37
KARATAEVA OLGA V., postgraduate student of the Department of endocrinology and internal medicine of Nizhny Novgorod State Medical Academy, Russia, 603000, Nizhny Novgorod, Malaya Pokrovskaya str., 12
PANOVA ELENA I., D. Med. Sci., professor of the Department of endocrinology and internal medicine of Nizhny Novgorod State Medical Academy, Russia, 603000, Nizhny Novgorod, Malaya Pokrovskaya str., 12
MOROZOVA ELENA P., C. Med. Sci., associate professor of the Department of endocrinology and internal medicine of Nizhny Novgorod State Medical Academy, Russia, 603000, Nizhny Novgorod, Malaya Pokrovskaya str., 12
ZHDANKINA NATALYA V., C. Med. Sci., assistant of professor of the Department of endocrinology and internal medicine of Nizhny Novgorod State Medical Academy, Russia, 603000, Nizhny Novgorod, Malaya Pokrovskaya str., 12
KOVALYOVA ALLA O., postgraduate student of the Department of endocrinology and internal medicine of Nizhny Novgorod State Medical Academy, Russia, 603000, Nizhny Novgorod, Malaya Pokrovskaya str., 12
KARPUNINA OKSANA N., interim of Head of the Medical Care unit of the Ministry of Internal Affairs of Russia in Nizhny Novgorod region, Russia, 603000, Nizhny Novgorod, Malaya Pokrovskaya str., 12, tel. (831) 268-69-05
PETROV SERGEY A., Head of the Hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in Nizhny Novgorod region, Russia, 603000, Nizhny Novgorod, Malaya Pokrovskaya str., 12, tel. +7-903-606-24-86, e-mail: gospital.mschmvd.52@gmail.ru ;
Abstract. Aim. The incidence of risk of sleep apnea syndrome development in working age patients suffering from arterial hypertension with normal body weight or obese has been revealed. In addition, analysis of interrelation between the risk of sleep apnea syndrome development and some anthropometric, laboratory and instrumental indicators, has been performed. Material and methods. Working age men with normal body weight or obese, suffering from arterial hypertension have been enrolled into the study. The risk of sleep apnea syndrome development has been assessed according to the questionnaire of Centre of sleep medicine at Barvikha health resort. According to the test results the patients have been divided into the groups with low, moderate and high risk. Moreover, lipid profile analyses, daily ECGmonitoring, echocardiography have been performed according to standard protocol. Results and discussion. High risk of sleep apnea syndrome development in patients with arterial hypertension was associated with a degree of obesity, signs of metabolic syndrome, hypercholesterolemia, hypertriglyceridemia and high atherogenic index. Morphological and functional parameters of myocardium in that group of patients are characterized by liability to tachycardia and premature beats; left ventricular diastolic dysfunction, interventricular septum hypertrophy and left atrium dilatation development. Consideration of those characteristics helps to estimate prognosis for that group of patients. Conclusion. Overweight, obese patients or the ones having metabolic syndrome are at high risk of sleep apnea syndrome development. The most significant laboratory and instrumental indicators in the group with the high risk of sleep apnea syndrome development were: atherogenic dyslipidemia, liability to arrhythmia, left ventricular diastolic dysfunction, left ventricular myocardium remodeling and left atrium dilatation.
Key words: sleep apnea syndrome, obesity, arterial hypertension.
For reference: Karataeva OV, Panova EI, Morozova EP, Zhdankina NV, Kovalyova AO, Karpunina ON, Petrov SA. The risk of sleep apnea syndrome development and its adverse cardiovascular effects in working age patients suffering from arterial hypertension with normal body weight or obese. The Bulletin of Contemporary Clinical Medicine. 2017; 10 (4): 32—37. DOI: 10.20969/ VSKM.2017.10(4).32-37.
Refereneces
- Fadeeva MI, Savelyeva LV, Fadeev VV. Syndrom obstruktivnogo apnoe sna v praktike vracha-endokrinologa [Obstructive sleep apnea syndrome in practice of endocrinologist]. Ozhirenie i metabolism [Obesity and metabolism]. 2010; 1: 3-10.
- Kallistov DU, Semenov VN, Romanov AI, Belov AM. Resultaty monitorirovaniya arterialnogo davlenia u pacientov s syndromom obstruktivnogo apnoe sna [Results of BP monitoring in patients with obstructive sleep apnea syndrome]. Kremljovskaya medicina; Klinicheskiy vestnik [«Kremljovskaya Medicina; Clinichesky Vestnik»]. 1998; 2: 38-42.
- Buzunov RV, Legeyda IV, Careva EV. Hrap I syndrom obstruktivnogo apnoe sna u vzroslyh I detey: practicheskoje posobie dlya vrachey [Snoring and obstructive sleep apnea syndrome in adult and children: practical guide for doctors]. Moscow. 2013; 170 p.
- Golubeva AA, Silvestrova GA. Lechenie narusheniy serdechnogo rytma i provodimosti pri syndrome obstruktivnogo apnoe sna [Cardiac arrhythmias and conducting disturbances treatment in obstructive sleep apnea syndrome]. Lechebnoje delo [Lechebnoje delo]. 2010; 3: 91–96.
- Popova MD, Kalinkin AL. Kachestvo zhizny i taktika vedeniya pacientov s narusheniyami rytma i provodimosti serdca, associirovannymi s syndromom obstruktivnogo apnoe sna [Quality of life and tactics of managing patients with disturbances of rhythm and conductivity of the heart asoociated with obstructive sleep apnea syndrome]. Medicinskiy vestnik Bashkortostana [Medical bulletin of Bashkortostan].2013; 8 (6): 192-194.
- Roche F, Xuong AN, Court-Fortune I, Costes F, et al. Relationship among the severity of sleep apnea syndrome, cardiac arrhythmias, and autonomic imbalance. Pacing Clin Electrophysiol. 2003; 26: 669–677.
- Balabanovich TI, Shyshko VI. Klinicheskaya i prognosticheskaya znachimostj syndroma obstruktivnogo apnoe/ gypopnoe sna u pacientov c neclapannoy fibrillyatsiey predserdiy [Clinical and prognostic significance of obstructive sleep apnea syndrome in patient with nonvalvular atrial fibrillation]. Zhurnal Grodnenskogo gosudarstvennogo medicinskogo universiteta [Grodno State Medical university journal]. 2016; 4: 12-19.
- Ivanov AP, Klyukvin DV, Rostorotskaya VV, Elgardt IA. Syndrom obstruktivnogo apnoe vo vremya sna u bolnyh ostrym infarctom myocarda: factory riska i effektivnostj lecheniya [Obstructive sleep apnea syndrome in patients with acute myocardial infarction: risk factors and effectiveness of treatment]. Klinicheskaya medicina [Clinical medicine]. 2012; 12: 27-30.
- Phillips BG, Somers VK. Sleep disordered breathing and risk factors for cardiovascular disease. Curr Opin Pulm. Med. 2002; 8: 516–520.
- Wolk R, Somers V. Cardiovascular consequences of obstructive sleep apnea. Clin Chest Med. 2003; 24: 195–205.
- Palman AD. Syndrom obstruktivnogo apnoe sna v praktike terapevta [Obstructive sleep apnea syndrome in therapeutic practice]. Effectivnaya farmakoterapiya [Effective pharmaco therapy]. 2013; 12: 46-54.
- Yaggi H, Mohsenin V. Sleep-disordered breathing and stroke. Clin Chest Med. 2003; 24: 223–237.
- Sviryaev UV, Korostovceva LS, Zvartau NE, Kalinkin AL, et al. Prognoticheskoje znachenie syndroma obstruktivnogo apnoe vo sne: promezhutochnye resultaty pjatiletnego prospectivnogo nabludenia [Prognostic significance of obstructive sleep apnea syndrome]. Arterialnaya hypertensia [Arterial hypertension]. 2011; 17 (1): 10-16.
- Lindberg E. Epidemiology of OSA. Respiratory Society Monograph. 2010; 50: 51-68.
- Shamsheva DS. Syndrom obstruktivnogo apnoe sna: sovremennoje sostoyanie problemy [Obstructive sleep apnea syndrome: modern state of the problem]. Lechebnoje delo [Lechebnoje delo]. 2014; 1: 4-16.
- Strueva NV, Poluectov MG, Saveljeva LV, Melnichenko GA. Ozhirenije i metabolism [Obesity and metabolism]. 2013; 3: 11-18.
- Strueva NV, Melnichenko GA, Poluectov MG, Saveljeva LV, et al. Gormonalnyi status i oreksinovaja sistema u bolnyh ozhireniem, oslozhnennym syndromom obstruktivnogo apnoe sna [Hormonal status and the orexin system in obese patients with obstructive sleep apnea syndrome]. Ozhirenije i metabolism [Obesity and metabolism]. 2015; 2: 24-30.
- Galyavi RA. Syndrom obstruktivnogo apnoe sna. Opredelenie, diagnostica, lechenie [Obstructive sleep apnea syndrome. Definition, diagnosis, treatment]. Vestnik sovremennoj klinicheskoj mediciny [The Bulletin of Contemporary Clinical Medicine]. 2010; 3 (4): 3842.
- Obstructive sleep apnea testing [Electronic resources]. http://www.sleepnet.ru/test-na-apnoe-sna/
- Orlov VN. Rucovodstvo po electrocardiographiy [Complete handbook on ECG]. Мoskva [Moscow]: «МIА». 2017; 560 p.
 THE FEATURES OF HORMONE METABOLIC PARAMETERS IN MEN WITH ARTERIAL HYPERTENSION ASSOCIATED WITH ANDROID OBESITY
THE FEATURES OF HORMONE METABOLIC PARAMETERS IN MEN WITH ARTERIAL HYPERTENSION ASSOCIATED WITH ANDROID OBESITY
UDC 616.12-008.331.1-056.257-008.9
DOI: 10.20969/ VSKM.2017.10(4).37-43
KOVALYOVA ALLA O., postgraduate student of the Department of endocrinology and internal medicine of Nizhny Novgorod State Medical Academy, Russia, 603000, Nizhny Novgorod, Malaya Pokrovskaya str., 12
PANOVA ELENA I., D. Med. Sci, professor of the Department of endocrinology and internal medicine of Nizhny Novgorod State Medical Academy, Russia, 603000, Nizhny Novgorod, Malaya Pokrovskaya str., 12
MOROZOVA ELENA P., C. Med. Sci., associate professor of the Department of endocrinology and internal medicine of Nizhny Novgorod State Medical Academy, Russia, 603000, Nizhny Novgorod, Malaya Pokrovskaya str., 12
ZHDANKINA NATALYA V., C. Med. Sci., assistant of professor of the Department of endocrinology and internal medicine of Nizhny Novgorod State Medical Academy, Russia, 603000, Nizhny Novgorod, Malaya Pokrovskaya str., 12
KARPUNINA OKSANA N., interim of Head of the Medical Care unit of the Ministry of Internal Affairs of Russia in Nizhny Novgorod region, Russia, 603000, Nizhny Novgorod, Malaya Pokrovskaya str., 12, tel. (831) 268-69-05
PETROV SERGEY A., Head of Hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in Nizhny Novgorod region, Russia, 603000, Nizhny Novgorod, Malaya Pokrovskaya str., 12, tel. +7-903-606-24-86, fax (831) 269-69-44, e-mail: gospital.mschmvd.52@gmail.com ;
Abstract. Aim. Study of clinical and laboratory features of arterial hypertension in working age male law enforcement officers with android obesity compared to patients without excessive body mass has been performed. Metabolic risk factors in arterial hypertension and their correlation with daily blood pressure monitoring parameters have been revealed. The efficiency of hypotensive treatment in real cardiologic practice has been evaluated. Material and methods. Male law enforcement officers have been enrolled into the study. The first group consisted of patients with arterial hypertension and android type of obesity. The representatives of the second group with arterial hypertension had normal body mass. All hospital patients have undergone clinical target organ examination and assessment of hypotensive therapy effectiveness. Besides complete clinical testing, detailed anthropometric measurements, 24hour blood pressure monitoring, biochemical and hormone analyses, including fasting glycemia, serum creatinine, hepatic transaminases, lipid profile and basal insulin have been performed with calculation of insulin resistance index. Results and discussion. Comparative analysis has shown significant differences between the groups in terms of some anthropometric data, more prominent changes in carbohydrate and lipid metabolism, biochemical signs of fatty hepatosis, hyperinsulinemia and high index of insulin resistance in patients with obesity. Identified hormone and metabolic disturbances have shown significant straight interrelation with some blood pressure monitoring parameters, reflecting unfavorable prognostic effects of progression and deterioration of arterial hypertension. However, comparative analyses of daily blood pressure profile didn’t reveal higher indicators in obesity group. It can be attributed to the greater number of hypotensive medications taken in hospital by the patients in this group. Conclusion. Hormone and metabolic factors should be noted among adverse factors associated with arterial hypertension and android type of obesity in working age males, such as: fasting hyperglycemia, atherogenic hyperlipidemia, elevation of hepatic transaminases, significant hyperinsulinemia and insulin resistance, that have shown more prominent changes in higher levels of blood pressure. More intensive hypotensive therapy is required in order to perform high quality treatment of arterial hypertension in working age males with android obesity.
Key words: arterial hypertension, android obesity, hormone and metabolic features.
For reference: Kovalyova AO, Panova EI, Morozova EP, Zhdankina NV, Karpunina ON, Petrov SA. The features of hormone metabolic parameters in men with arterial hypertension associated with android obesity. The Bulletin of Contemporary Clinical Medicine. 2017; 10 (4): 37—43. DOI: 10.20969/ VSKM.2017.10(4).37-43.
Refereneces
- Davhale RA, Potapova MV, Amirov NB. Rasprostranennost arterialnoy hypertensii sredi sotrudnikov pravoohranitelnyh organov [Prevalence of arterial hypertension among policemen]. Vestnik sovremennoj klinicheskoj mediciny [The Bulletin of Contemporary Clinical Medicine]. 2013; 6 (2): 66-72.
- Davidovich EM, Afonaskov OV, Kozyrenko AV, Staroverova UK. Rasprostranennost arterialnoy hypertonii I factorov riska u muzhchin molodogo i srednego vozrasta — voennoslyzhashih dalnevostochnogo voennogo [Prevalence of arterial hypertension and risk factors in young and middle-aged military man in Far East]. Dalnevostochnyj medicinskij jurnal [Far East medical journal]. 2008; 3: 10-13.
- Philippov EV. Arterialnaya hypertensia: kak optimizirovat terapiju pacienta? [Arterial hypertension: how to optimize therapy?]. Zemskyj vrach [Country doctor ]. 2015; 1 (25): 13-19.
- Roberie DR, Elliott WJ. What is the prevalence of resistant hyperetension in the United States? Curr Opin Cardiol. 2012; 27 (4): 386–391.
- Kearney P, Whelton M, Reynolds K, Whelton PK, et al. Worldwide prevalence of hypertension: a systematic review. Journal of Hypertension. 2004; 22 (1): 11–19.
- Lloyd-Jones D, Adams RJ, Brown TM, et al. Heart disease and stroke statistics — 2014 update: A report from the American Heart Association. Circulation. 2014; 129: 28–292.
- Bojcov SA, Balanova UA, Shalnova SA, Deev AD, et al. Arterialnaya hypertonia sredi lic 25-64 let: rasprostranennost, osvedomljonnost, lechenie i control; Po materialam issledovanija ESSE. [Arterial hypertension among individuals of 25-64 years old: prevalence, awareness, treatment and control; By the data from ECCD]. Kardiovasculyarnaja terapija i profilaktika [Cardiovascular therapy and Prevention].2014; 13 (4): 4–14.
- Chazova IE, Zhernakova UV, Oshepkova EV, Shalnova SA, et al. Rasprostranennost factorov riska serdechnososudistyh zabolevaniy v rossiyskoy populyacii bolnyh arterialnoy hypertoniey [Prevalence of cardiovascular diseases risk factors in Russian population with arterial hypertension]. Kardiologia [Cardioilogy].2014; 10: 4-12.
- Kaplan NM. The deadly quartet: Upper body obesity, glucose intolerance, hypertriglyceridemia, and hypertension. Arch Intern Med. 1989; 149: 1514–1520.
- Gerasimova AS, Oleynikov VE. Arterialnaya hypertoniya, associirovannaya s metabolicheskim syndromom: osobennosti techeniya i porazhenia organov-misheney [Arterial hypertension in association with metabolic syndrome: characteristics of clinical course and changes of target organs]. Izvestiya vysshyh uchebnyh zavedeniy; Povolzhskiy region [University proceedings; Volga region]. 2008; 3: 88-101.
- Kalashnikova MF. Metabolicheskiy syndrome: sovremennyi vzglyad na koncepciu, metody profilaktiki i lecheniya [Metabolic syndrome: a modern view on concept, prevention methods and treatment]. Effektivnaya farmakoterapiya: Endokrinologia [Effective pharmacotherapy: Endocrinology]. 2013; 55 (6): 52-63.
- Krasilnikova EI, Baranova EI, Blagosklonnaya YaV, Bystrova AA, et al. Mehanizmy razvitiya arterialnoy hypertenzii u bolnyh metabolicheskim syndromom [Mechanisms of arterial hypertension in metabolic syndrome] Arterialnaya hypertenziya [Arterial hypertension]. 2011; 17 (5): 405-414.
- Resistant Hypertension: Diagnosis, Evaluation and Treatment. A Scientific Statement From the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research (trans.A.O Konradi). Arterial hypertension. 2008; 14 (3): 187-202.
- Fendrikova AV, Skibitsky VV, Garkusha ES. Gendernye razlichia antihypertenzivnoy effektivnosti kombinirovannoy farmakoterapii u pacientov s refrakternoy arterialnoy hypertenziey i abdominalnym ozhireniem s uchetom solechuvstvitelnosti [Gender differences in antihypertensive efficiency of combination pharmacotherapy in patients with resistant hypertension and abdominal obesity in relation to salt sensitivity]. Arterialnaya hypertenziya. [Arterial hypertension]. 2016; 22 (4): 370-381.
- Krasilnikova EI, Blagosklonnaya YaV, Bystrova AA, Baranova EI, et al. Adipozopatiya — kluchevoe zveno razvitiya insulinoresistentnosti [Adiposopathy as a key factor in the development of insulin resistance]. Arterialnaya hypertenziya. [Arterial hypertension]. 2012; 18 (2): 165-176.
- Reaven GM. Insulin resistance / compensatory hyperinsulinemia, essential hypertension, and cardiovascular disease. J Clin Endocrinol Metab. 2003; 88: 2399–2403.
- Krasilnikova EI, Bystrova AA, Chilashvili MA, Stepanova VL, et al. Ozhirenie i angiotenzinII [Obesity and angiotensin II]. Arterialnaya hypertenziya. [Arterial hypertension]. 2013; 19 (3): 196-203.
- Kurshakova LN, Shabanova GJ, Sharifullina ER, Lysenko RG. Insulinoresistentnost i narusheniya uglevodnogo obmena pri metabolicheskom syndrome u muzhchin [Insulin resistance and carbohydrate metabolism disorders in metabolic syndrome in males]. Kazanskiy medicinskiy zhurnal [Kazan medical journal]. 2009; 90 (2): 239-243.
- Sergeeva VV, Rodionova AYu, Mikhailov AA, Bobyleva TA, et al. Principy antihypertenzivnoy terapii pri metabolicheskom syndrome [Principles of antihypertensive therapy in metabolic syndrome]. Klinicheskaya medicina [Clinical medicine]. 2013; 6: 4-8.
- Kremneva LV, Abaturova OV, Shalaev SV. Osobennosti antihypertenzivnoy terapii u bolnyh metabolicheskim syndromom [The features of antihypertensive therapy in patients with metabolic syndrome]. Racionalnaya farmakoterapiya v kardiologii [Ration Pharmacother Cardiol]. 2014; 10 (2): 212-219.
 RESULTS OF TREATMENT OF CHRONIC ISCHEMIA OF THE LOWER LIMBS
RESULTS OF TREATMENT OF CHRONIC ISCHEMIA OF THE LOWER LIMBS
UDC 617.58-005.4-036.12-089.168
DOI: 10.20969/VSKM.2017.10(4).43-47
MIROLYUBOV BORIS M., C. Med. Sci., associate professor of the Department of surgical diseases № 1 of Kazan State Medical University, Russia, 420012, Kazan, Butlerov str., 49; counselor of the Departments of vascular surgery № 1 and № 2 of Republic Clinical Hospital of the Ministry of Health of the Republic of Tatarstan; аngiosurgeon of the Department surgical of Clinical hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan, Russia, 420059, Kazan, Orenburg tract str., 132, tel. (843) 291-26-88
KAMALTDINOV RUSLAN R., student of Kazan State Medical University, Russia, 420012, Kazan, Butlerov str., 49
SAYFUTDINOVA ALINA R., student of Kazan State Medical University, Russia, 420012, Kazan, Butlerov str., 49
AGEEV ALEXANDER G., Head of the Department of surgical of Clinical hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan, Russia, 420059, Kazan, Orenburg tract str., 132, tel. (843) 291-26-88
GIMADIEV YUNUS F., surgeon of the Department of surgical of Clinical hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan, Russia, 420059 Kazan, Orenburg tract str., 132, tel. (843) 291-26-88
SAKHIBULLIN RAMIL F., Head of the endoscopy office of Clinical hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan, Russia, 420059, Kazan, Orenburg tract str., 132, tel. (843) 291-26-88, e-mail: sahibullin@mail.ru
FATTAKHOV SALIKH R., doctor of the Department of surgical of Clinical hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan, Russia, 420059, Kazan, Orenburg tract str., 132, tel. (843) 291-26-88
Abstract. Aim. Comparative analysis of effectiveness of treatment as well as of complications in patients who have undergone various shunt procedures for chronic arterial insufficiency of the lower limbs (femoropopliteal bypass and deep femoropopliteal bypass) was performed. Material and methods. The results obtained from 415 patients aged 40 to 90 years suffering from chronic arterial insufficiency of the lower limbs after the surgical treatment at Republic Clinical Hospital of the Ministry of Health of the Republic of Tatarstan in the department of vascular surgery number 1, were studied. The first group consisted of 329 patients who underwent autovenous femoropopliteal shunting. The second group consisted of 86 patients who underwent autovenous deep femoropopliteal shunting. Results and discussion. The effectiveness of treatment with autovenous femoropopliteal shunting was 76,6% (250 cases). In case of autovenous deep femoropopliteal shunting the efficacy was 92% (79 cases). In the first group of patients who underwent femoropopliteal shunting, complications occurred in 22% of cases. In the second group of patients who underwent deep femoropopliteal shunting, complications were seen in 8% of cases. The primary patency in femoropopliteal shunts in the early postoperative period was 98%, while the secondary patency was 99,6%. Primary patency in deep femoropopliteal shunting was 99%, while the secondary patency was 100%. Conclusion. Autovenous deep femoropopliteal shunting has a convincing advantage over autovenous femoropopliteal shunting in terms of effectiveness of treatment in the nearest postoperative period.
Key words: autovenous deep femoropopliteal shunting, autovenous femoropopliteal shunting, complications.
For reference: Mirolyubov BM, Kamaltdinov RR, Sayfutdinova AR, Ageev AG, Gimadiev YF, Sakhibullin RF, Fattachov SR. Results of treatment of chronic ischemia of the lower limbs. The Bulletin of Contemporary Clinical Medicine. 2017; 10 (4): 43—47. DOI: 10.20969/ VSKM.2017.10(4).43-47.
Refereneces
- Gorbenko MJu. Hirurgicheskoe lechenie ostryh trombozov arterij nizhnih konechnostej [Surgical treatment of acute thrombosis of the arteries of the lower extremities]. Moskva [Moscow]. 2010; 125 p.
- Pokrovskiy AV ed. Klinicheskaja angiologija: rukovodstvo [Clinical Angiology: а Handbook]. Moskva: Izdatel’stvo «Medicina» [M: Public Corporation “Medicine”). 2004; 2: 57-58.
- Bokerija LA ed. Perifericheskie arterii; Klinicheskie rekomendacii po vedeniju pacientov s sosudistoj arterial’noj patologiej: rossijskij soglasitel’nyj dokument [Peripheral arteries; Clinical recommendations for management of patients with cardiovascular arterial pathology: the Russian agreement]. Moskva: Izdatelstvovo NCSSH imeni AN Bakuleva RAMN [Moscow: Publishing House them AN Bakuleva RAMS)]. 2010; 1: 121 p.
- Nastavsheva O, Koshkin V, Dergacheva L. Kompleksnaja terapija obliterirujushhego ateroskleroza arterij nizhnih konechnostej [Complex therapy of obliterating athero- sclerosis of arteries of lower extremities]. Vrach [Doctor]. 2008; 7: 61-66.
-
Lysenko ER. Hirurgicheskoe lechenie bol’nyh s okkljuzi- onno-stenoticheskim porazheniem arterij goleni [Surgical treatment of patients with an occlusive-stenotic lesion of the lower leg arteries]. Moskva [Moscow]. 2012; 220 p.
-
Murav’eva JaJu. Takticheskie oshibki v lechenii bol’nyh s kriticheskoj ishemiej pri rekonstrukcii arterii nizhe pupartovoj svjazki [Tactical errors in the treatment of patients with critical ischemia in the reconstruction of the artery below the paunch ligament]. Moskva [Moscow]. 2014; 101 p.
-
Myshljonok DF. Rol’ gibridnyh tehnologij v lechenij pacientov s mnogojetazhnym ateroskleroticheskim porazheniem arterij nizhnih konechnostej [The role of hybrid technologies in the treatment of patients with multistory atherosclerotic lesions of the lower limb arteries]. Novosti hirurgii [Surgery News]. 2011; 19 (5): 67-73.
-
Conte MS. Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) and the (hoped for) dawn of evidence- based treatment for advanced limb ischemia. J Vasc Surg. 2010; 51 (Suppl. S): 69–75.
-
Glantz SA ed. Primer of biostatistics fourth edition. McGRAW-HILL Health Professions Division. 1994; 139–149.
 EXPERIENCЕ OF ORGANIZATION OF REHABILITATION TO COMBATANTS AT THE MEDICAL CARE UNIT OF THE MINISTRY OF INTERNAL AFFAIRS IN THE REPUBLIC OF BASHKORTOSTAN
EXPERIENCЕ OF ORGANIZATION OF REHABILITATION TO COMBATANTS AT THE MEDICAL CARE UNIT OF THE MINISTRY OF INTERNAL AFFAIRS IN THE REPUBLIC OF BASHKORTOSTAN
UDC 616-057.36-036.8:614.212(470.57)
DOI: 10.20969/ VSKM.2017.10(4).47-52
NAUSHIRVANOV OLEG R., Head of the Medical Care unit of the Ministry of Internal Affairs of Russia in Republic of Bashkortostan, Russia, 450015, Ufa, K. Marx str., 59
FAZLYEV MARAT M., D. Med. Sci., professor, Head of the Hospital of Medical Care unit of the Ministry of Internal Affairs of Russia in Republic of Bashkortostan, Russia, 450015, Ufa, K. Marx str., 59
NIGMATULLIN RUSTEM KH., C. Med. Sci., deputy Head of the Medical Care unit of the Ministry of Internal Affairs of Russia in Republic of Bashkortostan, Russia, 450015, Ufa, K. Marx str., 59, e-mail: nigrustem@yandex.ru
KUTUEV ZEMFIR Z., C. Med. Sci., deputy Head of the Medical Care unit of the Ministry of Internal Affairs of Russia in Republic of Bashkortostan, Russia, 450015, Ufa, K. Marx str., 59, e-mail: doczem@mail.ru
MIKHALEVA OLGA O., C. Med. Sci., Head of the Department of rehabilitation of Hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in Republic of Bashkortostan, Russia, 450015, Ufa, K. Marx str., 59, e-mail: fock20051@mail.ru
NAGAEVA REZEDA R., psychotherapist of the Department of rehabilitation of Hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in Republic of Bashkortostan, Russia, 450015, Ufa, K. Marx str., 59
Abstract. Fulfillment of combat and operational-service tasks in extreme conditions by employees of the Ministry of Internal Affairs allows anticipating development of numerous medical and psychological consequences. Aim. Results of rehabilitation activities in combatants performed at the Medical Unit of the Ministry of internal affairs of Russia in the republic of Bashkortostan have been analyzed. Material and methods. For the period of 2015—2016 2407 people were treated in rehabilitation center at the hospital of Medical unit of the Ministry of Internal Affairs of Russia in the Republic of Bashkortostan. All patients have undergone a complex examination. Personalized differentiated therapy for primary and concomitant diseases including physiotherapy and psychological correction, has been administered taking into account the symptoms of the phases of emotional burnout syndrome. Analysis of the work was carried out based on the annual report data and on the results of the Boyko questionnaire. Results and discussion. The work reflects the experience of dispensary and rehabilitation departments of the Medical unit of the Ministry of Internal Affairs of Russia in the Republic of Bashkortostan. Analysis of the survey results obtained from 386 combatants, who has undergone rehabilitation, was carried out. The article presents the principles and methods of work at dispensary and rehabilitation departments. It also reflects the main performance indicators. Conclusion. Positive results of the work testify the effectiveness of the ongoing rehabilitation program. The Medical unit of the Ministry of Internal Affairs of Russia in the Republic of Bashkortostan successfully implements rehabilitation programs for existing employees of internal affairs as well as for retirees of the Ministry of Internal Affairs.
Key words: medical rehabilitation, medical and psychological rehabilitation, rehabilitation treatment, individual rehabilitation program, emotional burnout syndrome.
For reference: Naushirvanov OR, Fazlyev MM, Nigmatullin RKh, Kutuev ZZ, Mikchaleva OO, Nagaeva RR. Experiencе of organization of rehabilitation to combatants at the medical unit of the ministry of internal affairs in the Republic of Bashkortostan. The Bulletin of Contemporary Clinical Medicine. 2017; 10 (4): 47—52. DOI: 10.20969/ VSKM.2017.10(4).47-52.
Refereneces
- Kubasov RV, Barachevskij YuE, Lupachev VV. Problemy professional’noj bezopasnosti sotrudnikov silovyh vedomstv — uchastnikov lokal’nyh vooruzhennyh konfliktov [Problems of the occupational safety of law enforcement officers — participants of local armed conflicts]. Mediko-biologicheskie i social’nopsihologicheskie problemy bezopasnosti v chrezvychajnyh situaciyah [Medico biological and socio psychological problems of safety in emergency situations]. 2014; 1: 39–46.
- Kubasov RV, Barachevskij YuE, Ivanov AM, Kubasova ED. Simpatoadrenalovaya i gipofizarno-nadpochechnikovaya aktivnost’ u sotrudnikov MVD Rossii pri razlichnyh urovnyah professional’noj napryazhennosti [Sympathoadrenal and pituitary-adrenal activity in the employees of the MIA of Russia with different levels of occupational tension].Ehkologiya cheloveka [Human Ecology]. 2015; 6: 9-14.
- Burenina IA, Iskhakova AN, Amirov NB, Sabirov LF. Opyt raboty otdeleniya reabilitacii Klinicheskogo gospitalya MSCH MVD RF po RT [Experience of the rehabilitation Department of the Clinical hospital of the medical unit of the interior Ministry in the Republic of Tatarstan]. Vestnik sovremennoj klinicheskoj mediciny [The Bulletin of Contemporary Clinical Medicine]. 2015; 8 (6): 135— 141.
- Ershova OYu. Programma psihologicheskoj reabilitacii sotrudnikov, vernuvshihsya iz sluzhebnoj komandirovki na territoriyu Severo-Kavkazskogo regiona [Program of psychological rehabilitation of employees returning from business trips on the territory of the North Caucasus region]. Psihopedagogika v pravoohranitel’nyh organah [Psychopedagogy in law enforcement bodies]. 2014; 2 (57): 99-102.
- Andreeva IA, Kuramshina LR. Issledovanie psihologicheskih osobennostej lic s PTSR [Study of the psychological characteristics of individuals with PTSD]. Nadѐzhnost’ deyatel’nosti v ehkstremal’nyh usloviyah [Dependability activities in extreme conditions]. 2005: 5–7.
- Kartashov VT. Sostoyanie sistemy dispanserizacii v Vooruzhennyh silah i napravlenie ee sovershenstvovaniya [The state of the system of medical examination in the Armed forces and the direction of its improvement]. Voenno-medicinskij zhurnal [Military medical journal]. 2007; 9: 27—29.
- Val’chuk EhA. Reabilitaciya i eѐ mesto v medicine [Rehabilitation and its place in medicine]. Medicinskaya reabilitaciya [Medical rehabilitation]. 2004; 1: 42-49.
- Pazhil’cev IV. Psihologicheskie osobennosti lichnosti sotrudnikov specpodrazdelenij MVD Rossii — uchastnikov kontrterroristicheskoj operacii na Severnom Kavkaze i ih psihoterapevticheskaya korrekciya [Psychological characteristics of employees of special forces of the Ministry of internal Affairs of Russia — participants of counterterrorist operation in the North Caucasus and their psychotherapeutic correction]. Sankt-Peterburg [Saint- Petersburg]. 2007; 20 p.
- Kalenov VA. Mediko-social’noe obosnovanie sovershenstvovaniya kompleksnoj reabilitacii uchastnikov boevyh dejstvij v sisteme vedomstvennogo zdravoohraneniya [Medical and social rationale for improving the comprehensive rehabilitation of participants of operations in the system of institutional health care]. Moskva [Moscow]. 2014; 164 p.
- Bochenkov AA, Glushko AN, Pulyko VI. Psihofiziologicheskie problemy professional’noj korrekcii i reabilitacii [Psychophysiological problems of professional correction and rehabilitation]. Voenno-medicinskij zhurnal [Military medical journal]. 2008; 6: 78–81.
- Bojko VV. Sindrom ehmocional’nogo vygoraniya v professional’nom obshchenii [Syndrome of emotional burnout in professional communication]. SPb: Piter [SPb: Peter]. 1999; 105 p.
 THE FACTORS OF CARDIOVASCULAR RISK IN MIDDLE AGED PATIENTS WITH ARTERIAL HYPERTENSION
THE FACTORS OF CARDIOVASCULAR RISK IN MIDDLE AGED PATIENTS WITH ARTERIAL HYPERTENSION
UDC 616.12-008.331.1-053.85-02
DOI: 10.20969/ VSKM.2017.10(4).53-58
OSHCHEPKOVA OLGA B., Head of the Department of cardiology of Clinical hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan, Russia, 420059, Kazan, Orenburg tract str., 132, e-mail: oschepkova.kazan@mail.ru
TCYBULKIN NIKOLAY A., C. Med. Sci., associate professor of the Department of cardiology, roentgen-endovascular and cardiovascular surgery of Kazan State Medical Academy — of the branch of Russian Medical Academy of Postgraduate Education, Russia, 420012, Kazan, Butlerov str., 36, e-mail: kldkgma@mail.ru
MIKHOPAROVA OLGA Y., Head of the Department of functional diagnostic of Clinical hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan, Russia, 420059, Kazan, Orenburg tract str., 132, e-mail: olga-mihoparova@rambler.ru
ABDRAKHMANOVA ALSU I., C. Med. Sci., associate professor of the Department of fundamental basis of clinical medicine of the Institute of Biology and Fundamental Medicine of Kazan Federal University, Russia, 420012, Kazan, K. Marx str., 74, e-mail: alsuchaa@mail.ru ;
Abstract. Aim. The features of cardiovascular risk factors in middle age patients with arterial hypertension without associated diseases have been defined. Material and methods. 60 patients with essential hypertension aged 28 to 60 have been examined. Diagnostic examination in hospital was sufficient to reveal or rule out symptomatic hypertension and combined cardiovascular pathology. Physical examination and history taking, complete blood count and biochemistry, common urine analysis, glomerular filtration rate, functional diagnostic examination, monitoring of clinical state in hospital have been performed. The signs of damage to target organs, the presence of modified risk factors of cardiovascular complications related to personal features and lifestyle, have been revealed and evaluated. The patients with associated disorders or serious inner organ diseases have not been enrolled to the study. Results and discussion. One of the leading factors of hypertension development in middle age is excess weight equally marked in all age groups. Common type of lipid metabolism disorder in middle-aged persons with hypertension is hypercholesterolemia. Essential factors of raising the stage of hypertension are age, excess weight and duration of hypertension. Conclusion. The leading factors for development of the disease in middle age patients with arterial hypertension are age, excess weight, lipid metabolism disorder and duration of hypertension. Non-smoking status is a favorable factor for the absence of associated diseases.
Key words: arterial hypertension, risk factors, age.
For reference: Oschepkova OB, Tcybulkin NA, Mihoparova OY, Abdrahmanova AI. The factors of cardiovascular risk in middle aged patients with arterial hypertension. The Bulletin of Contemporary Clinical Medicine. 2017; 10 (4): 53—58. DOI: 10.20969/ VSKM.2017.10(4).53-58.
Refereneces
- Jiang J, Zhang B, Zhang M, et al. Prevalence of conventional cardiovascular disease risk factors among Chinese Kazakh individuals of diverse occupational backgrounds in Xinjiang China. Int J Cardiol. 2015; 179: 558–560.
- Li W, Gu H, Teo K, et al. Hypertension prevalence, awareness, treatment, and control in 115 rural and urban communities involving 47 000 people from China. J Hypertens. 2016; 34: 39–46.
- Bhupathiraju SN, Hu FB. Epidemiology of Obesity and Diabetes and Their Cardiovascular Complications. Circ Res. 2016; 118: 1723–1735.
- Florczak E, Prejbisz A, Szwench-Pietrasz E, et al. Clinical characteristics of patients with resistant hypertension. J Hum Hypertens. 2013; 27: 678–685.
- Czernichow S, Castetbon K, Salanave B, et al. Determinants of blood pressure treatment and control in obese people: evidence from the general population. J Hypertens. 2012 Dec; 30 (12): 2338-2344.
- Sim JJ, Bhandari SK, Shi J, et al. Characteristics of resistant hypertension in a large, ethnically diverse hypertension population of an integrated health system. Mayo Clin Proc. 2013; 88: 1099–1107.
- Abdelmawgoud A, Brown CJ, Sui X, et al. Relationship of physical activity and healthy eating with mortality and incident heart failure among community-dwelling older adults with normal body mass index. ESC Heart Fail. 2015; 2: 20–24.
- Flegal KM, Kruszon-Moran D, Carroll MD, et al. Trends in Obesity Among Adults in the United States, 2005 to 2014. JAMA. 2016; 315: 2284–2291.
- Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 20112012. JAMA. 2014; 311: 806–814.
- Ghazi L, Oparil S, Calhoun DA, et al. Distinctive Risk Factors and Phenotype of Younger Patients With Resistant Hypertension: Age Is Relevant. Hypertension. 2017; https://doi.org/10.1161/HYPERTENSIONAHA.116.08632
- Jankowska-Polańska B, Chudiak A, Uchmanowicz I, et al. Selected factors affecting adherence in the pharmacological treatment of arterial hypertension. Patient Prefer Adherence. 2017; 11: 363-371.
- Hisamiev RSh, Amirov NB, Ginjatullina LR, Fatyhov NSh, Merikova EF, Jakimec SA. Sravnitel’nyj analiz zabolevaemosti arterial’noj gipertenziej i rasprostranennosti faktorov riska sredi sotrudnikov organov vnutrennih del Kazanskogo garnizona [Comparative analysis of the incidence of hypertension and of the prevalence of risk factors among internal affairs bodies of Kazan garrison]. Vestnik sovremennoj klinicheskoj mediciny [The Bulletin of Contemporary Clinical Medicine]. 2016; 9 (6): 89— 95.
 ANALYSIS OF THE ROLE OF ARTERIAL HYPERTENSION AND LIPID METABOLISM DISORDERS IN DEVELOPMENT AND PROGRESSION OF CHRONIC KIDNEY DISEASE IN PATIENTS WITH ESSENTIAL HYPERTENSION
ANALYSIS OF THE ROLE OF ARTERIAL HYPERTENSION AND LIPID METABOLISM DISORDERS IN DEVELOPMENT AND PROGRESSION OF CHRONIC KIDNEY DISEASE IN PATIENTS WITH ESSENTIAL HYPERTENSION
UDC 616.12-008.331.1-06:616.61-036.12
DOI: 10.20969/ VSKM.2017.10(4).58-64
SIGITOVA OLGA N., D. Med. Sci., professor, Head of the Department of general medical practice of Kazan State Medical University, Russia, 420012, Kazan, Butlerov str., 49, tel. (843)231-21-39, e-mail: osigit@rambler.ru
SHARIPOVA ROZALIA R., postgraduate student of the Department of general medical practice of Kazan State Medical University, Russia, 420012, Kazan, Butlerov str., 49, tel. (843)231-21-39, e-mail: sharipova.7@mail.ru
KIM TAISIYA YU., postgraduate student of the Department of general medical practice of Kazan State Medical University, Russia, 420012, Kazan, Butlerov str., 49, tel. (843)231-21-39, e-mail: tais_ariana@mail.ru
IBRAGIMOVA ALBINA A., resident of the Department of general medical practice of Kazan State Medical University, Russia, 420012, Kazan, Butlerov str., 49, tel. (843)231-21-39, e-mail: a.a.kayumova@bk.ru
FILINOVA MARINA A., resident of the Department of general medical practice of Kazan State Medical University, Russia, 420012, Kazan, Butlerov str., 49, tel. (843)231-21-39, e-mail: ma8672na@gmail.com ;
Abstract. Aim. The incidence of chronic kidney disease in patients with II-III stage arterial hypertension has been studied. The role of arterial hypertension in development of chronic kidney disease has been assessed by the indicators of stage, duration and onset of arterial hypertension. Lipid metabolism disorders were assessed by measurement of body mass index, determining hyper- and dyslipidemia. The rate of decline in progression of chronic kidney disease has been evaluated. Material and methods. 60 patients with II—III stage essential hypertension without concomitant cardiovascular diseases have been enrolled. Among those: 31 patient with chronic kidney disease and 29 — without it. Clinical examination, assessment of glomerular filtration rate as well as the decrease in glomerular filtration rate, albuminuria, lipid profile were carried out. Results and discussion. The incidence of chronic kidney disease in patients with 2—3 stage arterial hypertension without concomitant cardiovascular diseases was 9,0%. Among those, 54,8% of patient kidneys were affected by proteinuric type, and 45,2% — by non-proteinuric disease. Risk factors for kidney damage were the early onset, increased duration of arterial hypertension, increased systolic blood pressure, obesity, hyperlipidemia and dyslipidemia. Despite antihypertensive therapy carried out, the target level of arterial pressure has not been achieved in 11 (35,5%) of patients in group 1 and in 6 (20,7%) patients in group 2. The rate of chronic kidney disease progression evaluated by the decrease in glomerular filtration rate during a 3-year follow-up was (1,9±0,1) ml/min/year. Conclusion. Chronic kidney disease has been detected in 9% of patients with 2—3 stage arterial hypertension without concomitant cardiovascular diseases. The risk factors are the early onset and longer duration of arterial hypertension. In 45,2% patients secondary renal damage in essential hypertension belongs to non-proteinuric type. In 54,8% patients proteinuric variant is seen.
Key words: arterial hypertension, chronic kidney disease, glomerular filtration rate, albuminuria, hyperlipidemia.
For reference: Sigitova ON, Sharipova RR, Kim TYu, Ibragimova AA, Filinova MA. Analysis of the role of arterial hypertension and lipid metabolism disorders in development and progression of chronic kidney disease in patients with essential hypertension. The Bulletin of Contemporary Clinical Medicine. 2017; 10 (4): 58—64. DOI: 10.20969/ VSKM.2017.10(4).58-64.
Refereneces
- Xue JL, Ma JZ, Louis TA, Collins AJ. Forecast of the number of patients with end stage renal disease in the United States to the year 2010. J Am Soc Nephrol. 2001; 12 (12): 2753–2758.
- Meyer KB, Levey AS. Controlling the epidemic of cardiovascular disease in chronic renal disease: report from the National Kidney Foundation Task Force on cardiovascular disease. J Am Soc Nephrol. 1998; 9 (Suppl 12): 31–42.
- Preston RA, Singer I, Epstein M. Renal parenchymal hypertension: current concepts of pathogenesis and management. Arch Intern Med. 1996; 156 (6): 602–611.
- Guidelines Committee. 2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens. 2003; 21: 1011–1053.
- Hansson L, Zanchetti A, Carruthers SG, Dahlof B, Elmfeldt D, Julius S, Menard J, Rahn KH, Wedel H, Westerling S. Effects of intensive bloodpressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomized trial. Lancet. 1998; 351 (9118): 1755–1762.
- Pepine CJ, Kowey PR, Kupfer S et al. Predictors of adverse outcome among patients with hypertension and coronary artery disease. J Am Coll Cardiol. 2006; 47 (3): 547–551.
- Liu L, Zhang Y, Liu G, Li W, Zhang X, Zanchetti A, FEVER Study Group. The Felodipine Event Reduction (FEVER) Study: a randomized long-term placebo-controlled trial in Chinese hypertensive patients. J Hypertens. 2005; 23 (12): 2157–2172.
- Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies [published erratum appears in Lancet. 2003; 361(9362): 1060]. Lancet. 2002; 360 (9349): 1903-1913.
- UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998; 317 (7160): 703-713.
- Estacio RO, Jeffers BW, Gifford N, Schrier RW. Effect of blood pressure control on diabetic microvascular complications in patients with hypertension and type 2 diabetes. Diabetes Care. 2000; 23 (Suppl 2): 54–64.
- Casas JP, Chua W, Loukogeorgakis S et al. Effect of inhibitors of the renin-angiotensin system and other antihypertensive drugs on renal outcomes: systematic review and meta-analysis. Lancet. 2005; 366 (9502): 2026–2033.
- Kidney Disease Outcomes Quality Initiative (K/DOQI). K/DOQI clinical practice guidelines on hypertension, antihypertensive agents in chronic kidney disease. Am J Kidney Dis. 2004; 43(5 Suppl 1): 1–290.
- Levey AS, Greene T, Beck GJ et al. Dietary protein restriction and the progression of chronic renal disease: what have all of the results of the MDRD study shown? Modification of Diet in Renal Disease Study group. J Am Soc Nephrol. 1999; 10 (11): 2426–2439.
- Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R,Germano G, et al. 2007 ESH-ESC Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Blood Press. 2007; 16(3): 135-232.
- Mancia G, Fagard R, Narkiewicz K et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013; 34 (28): 2159-2219.
- Lewis JB. Blood pressure control in chronic kidney disease: is less really more? J Am Soc Nephrol. 2010; 21 (7): 1086–1092.
- Klahr S, Levey AS, Beck GJ et al. The effects of dietary protein restriction and blood-pressure control on the progression of chronic renal disease. Modification of Diet in Renal Disease Study Group. N Engl J Med. 1994; 330 (13): 877–884.
- Wright JT Jr, Bakris G, Greene T et al. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. JAMA. 2002; 288 (19): 2421–2431.
- Ruggenenti P, Perna A, Loriga G et al. Blood-pressure control for renoprotection in patients with nondiabetic chronic renal disease (REIN-2): multicentre, randomized controlled trial. Lancet. 2005; 365 (9463): 939–946.
- Appel LJ, Wright JT Jr, Greene T et al. Intensive bloodpressure control in hypertensive chronic kidney disease. N Engl J Med. 2010; 363 (10): 918–929.
- Cushman WC, Evans GW, Byington RP et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010; 362 (6): 1575–1585.
- Upadhyay A, Earley A, Haynes SM, Uhlig K. Systematic review: blood pressure target in chronic kidney disease and proteinuria as an effect modifier. Ann Intern Med. 2011; 154 (8): 541–548.
- Graham I, Atar D, Borch-Johnsen K et al. European guidelines on cardiovascular disease prevention in clinical practice: executive summary: Fourth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (Constituted by representatives of nine societies and by invited experts). Eur Heart J. 2007; 28 (19): 2375-2414.
- Volpe M, Battistoni A, Tocci G, et al. Cardiovascular risk assessment beyond systemic coronary risk estimation: a role for organ damage markers. J Hypertens. 2012; 30 (6): 1056–1064.
- Parving HH. Initiation and progression of diabetic nephropathy. N Engl J Med. 1996; 335 (22): 1682– 1683.
- Ninomiya T, Perkovic V, de Galan BE, Zoungas S, Pillai A, Jardine M, et al. Albuminuria and kidney function independently predict cardiovascular and renal outcomes in diabetes. J Am Soc Nephrol. 2009; 20 (8): 1813– 1821.
- Zanchetti A, Hansson L, Dahlof B, Elmfeldt D, Kjeldsen S, Kolloch R et al. Effects of individual risk factors on the incidence of cardiovascular events in the treated hypertensive patients of the Hypertension Optimal Treatment Study. HOT Study Group. J Hypertens. 2001; 19 (6): 1149–1159.
- Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009; 373 (9669): 10831096.
- Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013; 309 (1): 71–82.
- Chapman MJ, Ginsberg HN, Amarenco P et al. Triglyceriderich lipoproteins and high-density lipoprotein cholesterol in patients at high risk of cardiovascular disease: evidence and guidance for management. Eur Heart J. 2011; 32 (11): 1345–1361.
 DIAGNOSIS AND TREATMENT OF SLEEP BREATHING DISORDERS IN MEDICAL HOSPITAL PATIENTS
DIAGNOSIS AND TREATMENT OF SLEEP BREATHING DISORDERS IN MEDICAL HOSPITAL PATIENTS
UDC 616.24-008.444:616.12-008.331.1
DOI: 10.20969/ VSKM.2017.10(4).64-68
SMOLYANINOV SERGEY V., D. Med. Sci., professor of the Department of public health, economics and health management of N.N. Burdenko Voronezh State Medical University; Head of Hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Voronezh region, colonel of internal service, Russia, 394086, Voronezh, Patriotov ave., 52, e-mail: e-msch36@bk.ru
LYSHOVA OLGA V., D. Med. Sci., professor of the Department of internal medicine of N.N. Burdenko Voronezh State Medical University, Russia, 394036, Voronezh, Studencheskaya str., 10
KULAKOVA ANNA A., C. Med. Sci., Head of Hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Voronezh region, lieutenant colonel of internal service, Russia, 394086, Voronezh, Patriotov ave., 52
IVANNIKOVA LYUDMILA V., C. Med. Sci., Head of the Department of internal medicine of Hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Voronezh region, major of internal service, Russia, 394086, Voronezh, Patriotov ave., 52
KOSTENKO IRINA I., Head of the Department of rehabilitation of Hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Voronezh region, Russia, 394086, Voronezh, Patriotov ave., 52
KHARINA NATALYA V., C. Med. Sci., physician of the Department of internal medicine of Hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Voronezh region, Russia, 394086, Voronezh, Patriotov ave., 52
Abstract. Disorders of breathing regulation during sleep might be one of the reasons for recrudescence and progression of cardiovascular diseases. Apnea-hypopnea syndrome during sleep is characterized by complete (apnea) or partial (hypopnea) termination of airflow through the upper respiratory tract for 10 seconds or more. Aim. The frequency of sleep apnea-hypopnea detection in men with different stage essential hypertension and the dynamics of obstructive and central sleep apnea episodes during short-term non-invasive respiratory support have been studied. Material and methods. The objects of the research were men (n=334) aged 20—72 years [mean age (46,5±4,7) years] suffering from I, II and III stage hypertension undergoing examination and treatment at internal medicine and rehabilitation departments at the hospital of Medical Unit of the Ministry of Internal Affairs of Russia in the Voronezh Region in the period from 2011 to 2016. Results and discussion. The frequency of sleep apnea-hypopnea syndrome detection in patients (all male) with I-III stage hypertension was 82% from the 334 surveyed. Upon that obstructive type has been diagnosed in 96% of the cases, in 4% of the cases — central type. Short-term (from 1 to 12 nights) non-invasive respiratory support with positive air pressure was conducted in 58 (17%) patients. Significant obstructive apnea index reduction up to 5 episodes/ hour and less has been observed in the majority of patients. The treatment was ineffective only in 10 patients (6%) due to the central origin of apnea-hypopnea episodes. Conclusion. There is a high detectability of obstructive sleep apnea-hypopnea syndrome in patients with essential hypertension. More than half of the patients have moderate or severe degree of sleep apnea-hypopnea syndrome. Positive air pressure therapy was effective primarily in patients with obstructive respiratory disorders, whereas it turned ineffective in patients with periodic Cheyne-Stokes breathing and systolic dysfunction.
Key words: essential arterial hypertension, sleep apnea-hypopnea syndrome, men, non-invasive respiratory support.
For reference: Smolyaninov SV, Lyshova OV, Kulakova AA, Ivannikova LV, Kostenko II, Kharina NV. Diagnosis and treatment of sleep breathing disorders in medical hospital patients. The Bulletin of Contemporary Clinical Medicine. 2017; 10 (4): 64—68. DOI: 10.20969/ VSKM.2017.10(4).64-68.
Refereneces
- Naughton M, Benard D, Tam A et al. Role of hyperventilation in the pathogenesis of central sleep apneas in patients with congestive heart failure. Am Rev Respir Dis. 1993; 148 (2): 330–338.
- Hedner J, Ejnell H, Caidahl K. Left ventricular hypertrophy independent of hypertension in patients with obstructive sleep apnea. J Hypertens. 1990; 8: 941-946.
- Javaheri S, Parker TJ, Liming JD et al. Sleep apnea in 81 ambulatory male patients with stable heart failure; Types and their prevalences, consequences and presentations. Circulation. 1998; 97 (21): 2154-2159.
- Hermann DM, Bassetti CL. Sleep-related breathing and sleep-wake disturbances in ischemic stroke. Neurology. 2009; 73: 1313-1322.
- Logan AG, Perlikowski SM, Mente Aet al. High prevalence of unrecognized sleep apnoea in drug-resistant hypertension. J Hypertens. 2001; 19 (12): 2271-2277.
- Franklin KA, Nilsson JB, Sahlin C, Näslund U. Sleep apnoea and nocturnal angina. Lancet. 1995; 345 (8957): 1085-1087.
- Lee CH, Khoo SM, Tai BC et al. Obstructive sleep apnea in patients admitted for acute myocardial infarction: Prevalence, predictors, and effect on microvascular perfusion. Chest. 2009; 135 (6): 1488-1495.
- Hermann DM, Bassetti CL. Sleep-related breathing and sleep-wake disturbances in ischemic stroke. Neurology. 2009; 73: 1313-1322.
- Epstein LJ, Kristo D, Strollo PJJr et al. Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine: Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009; 5 (3): 263-276.
- Berry RB, Budhiraja R, Gottlieb DJ et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. J Clin Sleep Med. 2012; 8 (5): 597-619.
- Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002; 165 (9): 1217-1239.
 MODERN METHODICAL APPROACHES TO PLANNING THE NUMBER OF ATTENDING PHYSICIANS IN HEALTH RESORTS
MODERN METHODICAL APPROACHES TO PLANNING THE NUMBER OF ATTENDING PHYSICIANS IN HEALTH RESORTS
DOI:10.20969/VSKM.2017.10(4).68-73
SHIPOVA VALENTINA M., D. Med. Sci., professor, chief researcher worker of N. Semashko National Research Institute of Public Health, Russia, Moscow, Vorontzovo Pole str., 12, build 1, tel. +7-916-505-59-33, e-mail: vshipova@yandex.ru
GADZHIEVA SAIDA M., chief physician of Children’s Health Resort № 42 of Moscow Department of Health care, Russia, Moscow, Tamanskaya str., 15, block 2, tel. +7-903-499-199-28-25, e-mail: Sanatory42@gmail.com
BERSENEVA EVGENIA A., D. Med. Sci., Head of the Department of the higher and additional professional education of N. Semashko National Research Institute of Public Health, Russia, Moscow, Vorontzovo Pole str., 12, build 1, tel. +7-916-216-84-59, e-mail: eaberseneva@gmail.com ;
Abstract. Topical issues of planning the number of attending physicians in health resorts are considered in the article. Aim. Development of modern methodical approaches on planning the number of attending physicians in health resorts is being considered. Material and methods. The following methods were applied: statistical, economic, and analytical and calculation research methods of the expert and performance standards evaluation. Results and discussion. Modern methodical approaches to planning the number of attending physicians in health resorts were developed. Conclusion. The use of presented methodical approaches on planning the number of attending physicians in health resorts allows carrying out scientific justification of the performance standards. Besides, the technique can be widely used in pricing and economic analysis of institution activity. It is expedient to apply the materials in expert assessment of the amount of medical care when developing clinical protocols of treatment in health resorts.
Key words: work rationing, health resorts for children.
For reference: Shipova VM, Gadzhieva SM, Berseneva EA. Modern methodical approaches to planning the number of attending physicians in health resorts. The Bulletin of Contemporary Clinical Medicine. 2017; 10 (4): 68—73. DOI: 10.20969/VSKM.2017.10(4).68-73.
Refereneces
- Baranov AA. Nashacel’ — dobit’sja, chtobykazhdyjrebenok v Rossiiroszdorovymischastlivym [Our purpose — to achieve that each child in Russia of dews healthy and happy]. Vestnik Roszdravnadzora [Bulletin of Roszdravnadzor]. 2016; 3: 5-8.
- Starodubova VI, Shhepinaidr OP ed. Obshhestvennoe zdorov’e i zdravoohranenie: nacional’noe rukovodstvo [Public health and health care: national leaders]. Moskva [Moscow]: GJeOTAR-Media. 2013; 624 p.
- Baranov AA, Namazova-Baranova LS, Terleckaja RN, Bajbarina EN, Chumakova OV, Ustinova VN, Antonova EV, Vishneva EA. Rezul’taty profilakticheskih medicinskih osmotrov nesovershennoletnih v Rossijskoj Federacii [Results of routine medical examinations of minors in the Russian Federation]. Rossijskij pediatricheskij zhurnal [Russian pediatric magazine]. 2016; 19 (5): 287-293.
- Zelinskaja DI. Detskaja invalidnost’ (mediko-social’noe issledovanie) [Children’s disability (medico-social research)]. Moskva [Moscow]. 1998; 53 p.
- Zelinskaja DI, Terleckaja RN. Invalidnost’ detskogo naselenija Rossii [Disability of the children’s population of Russia]. Moskva: Centr razvitija mezhsektoral’nyh program [Moscow: Center for the Development of Intersectoral Programs]. 2008: 135–160.
- Polunina NV, Cherkasov SN. Osobennosti sostojanija zdorov’ja detej Rossijskoj Federacii i puti ego uluchshenija [Russian Federation children health state features and the way of it’s improvement]. Jakutsk: Prioritetnye napravlenija razvitija zdravoohranenija Dal’nego Vostoka i bajkal’skogo regiona — problemy i perspektivy [Yakutsk: Priority directions of health development in the Far East and the Baikal region — problems and prospects]. 2013; 203-207.
- Chicherin LP, Leshkevich IA, Mihal’skaja EV, Proshin VA. Problemy optimizacii medicinskogo obespechenija detej i podrostkov [Medical support of children and teenagers optimization problems]. Rossijskij pediatricheskij zhurnal [Russian pediatric magazine]. 2005; 4: 51-54.
- Chicherin LP, Nikitin MV. Mediko-social’nye aspekty ohrany zdorov’ja detej i podrostkov v Rossijskoj Federacii [Medico-social aspects of health protection of children and teenagers in the Russian Federation]. Obshhestvennoe zdorov’e i zdravoohranenie [Public health and health care]. 2010; 3: 22-26.
- Chicherin LP, Nikitin MV, Shhepin VO, Cherkashina IV. Sanatorno-kurortnaja pomoshh’ detjam v Rossii [Children sanatorium help in Russia]. Problemy social’noj gigieny, zdravoohranenija i istorii mediciny [Problems of social hygiene, health care and history of medicine]. 2015; 4: 3-6.
- Shhepin VO, Rastorgueva TI, Karpova OB. Sovremennye demograficheskie tendencii v Possijskoj Federacii [Current demographic trends in the Russian Federation]. Rossijskaja akademija medicinskih nauk: bjulleten’ Nacional’nogo nauchno-issledovatel’skogo instituta obshhestvennogo zdorov’ja [Russian academy of medical sciences: bulletin of National research institute of public health]. 2013; 2: 10-13.
 ETHNOS END OBSTRUCTIVE APNEA/HYPOPNEA SYNDROME (foreign literature review)
ETHNOS END OBSTRUCTIVE APNEA/HYPOPNEA SYNDROME (foreign literature review)
UDC [616.24-008.444:613.79]-054(048.8)
DOI: 10.20969/ VSKM.2017.10(4).74-80
GOLOKOV VLADISLAV A., C. Med. Sci., internal service major, Head of the Department of neurological of Hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Yakutia region, Russia, 677005, Yakutsk, Sverdlov str., 1/2, e-mail: yamchik@inbox.ru
SHNAYDER NATALIA A., D. Med. Sci., professor, Head of the Department of medical genetics and clinical neurophysiology of Postgraduate Education Institute of V.F. Voyno-Yasenetsky Krasnoyarsk State Medical University, Russia, 660022, Krasnoyarsk, Partisan Zheleznyak str., 1, e-mail: naschnaider@yandex.ru
NIKOLAEVA TATJANA YА., D. Med. Sci., professor, Head of the Department of neurology and psychiatry M.K. Ammosov Nord-East Federal University, Russia, 677000, Yakutsk, P. Alekseev str., 83а, e-mail: tyanic@mail.ru
DOLINSKAYA ELVIRA A., internal service colonel, Head of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Yakutia region, Russia, 677005, Yakutsk, Sverdlov str., 1/2, e-mail: mshmvdrsy@mail.ru
SOLOVYEVA SARDANA F., internal service lieutenant colonel, Head of Hospital, of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Yakutia region, Russia, 677005, Yakutsk, Sverdlov str., 1/2, e-mail: mshmvdrsy@mail.ru
GOLOKOVA ELENA A., neurologist of the Department of functional diagnostics of Republic Hospital № 2 — Center of emergency medicine, Russia, 677005, Yakutsk, P. Alekseev str., 83а, e-mail: ele-stars@mail.ru
ALEXEEVA OLGA V., therapist-somnologist of Neurological center of epileptology, neurogenetics and brain research of University clinic of V.F. Voyno-Yasenetsky Krasnoyarsk State Medical University, Russia, 660022, Krasnoyarsk, Partisan Zheleznyak str., 1, e-mail: aleksvrach@mail.ru
PAVLOV YEGOR M., internal service major, Head of the Department of the medical, preventative, organizational and methodical of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Yakutia region, Russia, 677005, Yakutsk, Sverdlov str., 1/2, e-mail: mshmvdrsy@mail.ru
EFREMOVA ANASTASIA I., neurologist of the military physician board of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Yakutia region, Russia, 677005, Yakutsk, Sverdlov str., 1/2, e-mail: mshmvdrsy@mail.ru ;
Abstract. The syndrome of obstructive sleep apnea/hypopnea is a common, life-threatening type of sleep apnea, which is caused by obstruction of the upper respiratory tract. This condition is characterized by repeated pauses in breathing during sleep, despite the efforts of respiratory muscles. It is usually associated with a decrease in blood oxygen saturation. The researchers are interested in this problem due to the fact that obstructive sleep apnea/hypopnea syndrome is an adverse consequence of cardiovascular diseases and sudden death. Aim. Analysis of modern data on prevalence, risk factors, pathogenesis, phenotypes, diagnosis and treatment of obstructive sleep apnea/hypopnea syndrome has been performed. Material and methods. The article provides an overview of research on the role of ethnos in development of this disease. Results and discussion. The data on prevalence, phenotypic differences, approaches to diagnostics and treatment of obstructive sleep apnea/hypopnea syndrome in different ethnic groups in the countries of America, Europe, and Asia is presented. Conclusion. Despite the comparable prevalence of obstructive sleep apnea/hypopnea syndrome in different ethnic groups, pathogenic factors leading to development of the disease are diverse and vary widely. Their separate dominance or combined representations probably have a genetic basis. The phenotypes and severity of obstructive sleep apnea/hypopnea syndrome vary among populations. Available clinical and instrumental screening examination of patients with obstructive sleep apnea/hypopnea syndrome in different ethnic groups allows identifying the degree of risk of this pathology in order to carry out timely prevention and correction.
Key words: obstructive sleep apnea, hypopnea, ethnos, phenotype, risk factor, review.
For reference: Golokov VA, Shnayder NA, Nikolaeva TY, Dolinskaya EA, Solovyeva SF, Golokova EA, Alexeeva OV, Pavlov YM, Efremova AI. Ethnos end obstructive apnea / hypopnea syndrome (foreign literature review). The Bulletin of Contemporary Clinical Medicine. 2017; 10 (4): 74—80. DOI: 10.20969/ VSKM.2017.10(4).74-80.
Refereneces
- Chan, A.S. Obstructive sleep apnea — an update / A.S. Chan, C.L. Phillips, P.A. Cistulli // Intern. Med. J. — 2010. — № 40. — P.102—106.
- Parish, J.M. Obstructive sleep apnea and cardiovascular disease/ J.M. Parish, V.K. Somers // Mayo. Clin. Proc. — 2004. — № 79. — P.1036—1046.
- Grundy, S.M. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement / S.M. Grundy, J.I. Cleeman, S.R. Daniels // Circulation. — 2005. — № 112. — P.2735—2752.
- Young, T. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort / T. Young, L. Finn, P.E. Peppard // Sleep. — 2008. — № 31 (8). — P.1071—1078.
- Association of psychiatric disorders and sleep apnea in a large cohort / A. Sharafkhaneh, N. Giray, P. Richardson [et al.] // Sleep. — 2005. — № 28. — P.1405—1411.
- George, C.F. Sleepiness, sleep apnea, and driving: still miles to go before we safely sleep / C.F. George // Am. J. Respir. Crit. Care Med. — 2004. — № 170. — P.927—928.
- Systematic review and meta-analysis of the literature regarding the diagnosis of sleep apnea / S.D. Ross, I.A. Sheinhait, K.J. Harrison [et al.] // Sleep. — 2000. — № 23 (4). — P.519—532.
- Lim, L.L. Obstructive sleep apnea in Singapore: polysomnography data from a tertiary sleep disorders unit The sleep of African Americans: a comparative review/ L.L. Lim, K.W. Tham, S.M. Fook-Chong // Ann. Acad. Med. Singapore. — 2008. — № 37 (8). — P.629—636.
- Occupational screening for sleep disorders in 12-h shift nurses using the Berlin Questionnaire / J. Geiger-Brown, V.E. Rogers, K. Han [et al.] // Sleep Breath. — 2013. — № 17 (1). — P.381—388.
- A community study of sleep-disordered breathing in middle-aged Chinese men in Hong Kong / M.S. Ip, B. Lam, I.J. Lauder [et al.] // Chest. — 2001. — № 119. — P.62—69.
- Kim, J. Prevalence of sleep-disordered breathing in middle-aged Korean men and women / J. Kim, K. In, K. Kang [et al.] // Am. J. Respir. Crit. Care Med. — 2004. — № 170. — P.1108—1113.
- Prevalence of snoring and witnessed apnea in Taiwanese adults / L.P. Chuang, S.C. Hsu, S.W. Lin [et al.] // Chang Gung Med. J. — 2008. — № 31. — P.175—181.
- Kamil, M.A. Snoring and breathing pauses during sleep in the Malaysian population / M.A. Kamil, C.L. Teng, S.A. Hassan // Respirology. — 2007. — № 12. — P.375—380.
- Epidemiology of sleep-related complaints associated with sleep-disordered breathing in Bangkok. Thailand / P. Suwanprathes, C. Won, C. Komoltri [et al.] // Sleep Med. — 2010. — № 11. — P.1025—1030.
- Obstructive sleep apnea-hypopnea syndrome patients with overweight and hypertension in a Japanese work place / K. Okabayashi, E. Kasahara, H. Uchiyama [et al.] // J. Occup. Health. — 2007. — № 49. — P.117—124.
- Prevalence and risk factors of obstructive sleep apnea among middle-aged urban Indians: a community-based study / E.V. Reddy, T. Kadhiravan, H.K. Mishra [et al.] // Sleep Med. — 2009. — № 10 (8). — P.913—918.
- Prevalence of symptom sand risk of sleep apnea in middleaged Saudi males in primary care / А.S. BaHammam, M.S. Alrajeh, H.H. Al-Jahdali [et al.] // Saudi. Med. J. — 2008. — № 29 (3). — P.423—426.
- Symptoms and risk of obstructive sleep apnea in primary care patients in Jordan / B. Khassawneh, M. Ghazzawi, Y. Khader [et al.] // Sleep Breath. — 2009. — № 13 (3). — P.227—232.
- Prevalence of sleep apnea-related symptoms in a Persian population / B. Amra, Z. Farajzadegan, M. Golshan [et al.] // Sleep Breath. — 2011. — № 15 (3). — P.425—429.
- Risk for sleep apnea syndrome in Pakistan: a crosssectional survey utilizing the Berlin questionnaire / F. Taj, Z. Aly, O. Arif [et al.] // Sleep Breath. — 2009. — № 13 (1). — P.103—106.
- Symptoms of obstructive sleep apnea in a Caribbean sample / F. Zizi, G. Jean-Louis, S. Fernandez [et al.] // Sleep Breath. — 2008. — № 12 (4). — P.317—322.
- Watanabe, T. Contribution of body habitus and craniofacial characteristics to segmental closing pressures of the passive pharynx in patients with sleep-disordered breathing / T. Watanabe, S. Isono, A.Tanaka // Am. J. Respir. Crit. Care Med. — 2002. — № 165. — P.260— 265.
- Фенотипические и генотипические факторы риска синдрома обструктивного апноэ/гипопноэ сна / Н.А. Шнайдер, И.А. Демко, О.И. Алексеева [и др.] // Проблемы женского здоровья. — 2015. — № 2, т. 10. — С.55—64. [Shnajder NA, Demko IA, Alekseeva OI, Petrova MM, Kantimirova EA, Strockaja IG, Djuzhakov SK. Fenotipicheskie i genotipicheskie faktory riska sindroma obstruktivnogo apnoje/gipopnoje sna [Phenotypic and genotypic risk factors for obstructive sleep apnea/ hypopnea sleep]. Problemy zhenskogo zdorov’ja [Women’s health Issues]. 2015; 2 (10): 55-64].
- Mirrakhimov, A.E. Prevalence of obstructive sleep apnea in Asian adults: a systematic review of the literature / A.E. Mirrakhimov, T. Sooronbaev, E.M. Mirrakhimov // Pulm. Med. — 2013. — DOI: 10.1186 / 1471-2466-13-10.
- Sakakibara, H. Cephalometric abnormalities in nonobese and obese patients with obstructive sleep apnea / H. Sakakibara, M. Tong, K. Matsushita [et al.] // Eur. Respir. J. — 1999. — № 13. — P.403—410.
- Central obesity and health-related factors among middleaged men: a comparison among native Japanese and Japanese-Brazilians residing in Brazil and Japan / A. Schwingel, Y. Nakata, L.S. Ito [et al.] // J. Physiol. Anthropol. — 2007. — № 26. — P.339—347.
- Thyroxine replacement therapy reverses sleep-disordered breathing in patients with primary hypothyroidism / A. Jha, S.K. Sharma, N. Tandon [et al.] // Sleep Med. — 2006. — № 7. — P.55—61.
- Schwab, R.J. Identification of upper airway anatomic risk factors for obstructive sleep apnea with volumetric magnetic resonance imaging / R.J.Schwab, M. Pasirstein, R. Pierson // Am. J. Respir. Crit. Care Med. — 2003. — № 168. — P.522—530.
- Obesity and obstructive sleep apnea: pathogenic mechanisms and therapeutic approaches / A.R. Schwartz, S.P. Patil, A.M. Laffan [et al.] // Proc. Am. Thorac. Soc. — 2008. — № 5. — P.185—192.
- Martins, A.B. Physiopathology of obstructive sleep apneahypopnea syndrome / A.B. Martins, S. Tufik, S.M. Moura // J. Bras. Pneumol. — 2007. — № 33. — P.93—100.
- Young, T. Excess weight and sleep-disordered breathing / T. Young, P.E. Peppard, S. Taheri // J. Appl. Physiol. — 2005. — № 99. — P.1592—1599.
- Hora, F. Clinical, anthropometric and upper airway anatomic characteristics of obese patients with obstructive sleep apnea syndrome / F. Hora, L.M. Napolis, C. Daltro // Respiration. — 2007. — № 74. — P.517—524.
- Simpson, L. Sex differences in the association of regional fat distribution with the severity of obstructive sleep apnea / L. Simpson, S. Mukherjee, M.N. Cooper // Sleep. — 2010. — № 33. — P.467—474.
- Neck circumference as a measure of central obesity: associations with metabolic syndrome and obstructive sleep apnea syndrome beyond waist circumference / A. Onat, G. Hergenç, H. Yuksel [et al.] // Clin. Nutr. — 2009. — № 28. — P.46—51.
- Obstructive sleep apnea syndrome and anthropometric obesity indexes / A.C. Soylu, E. Levent [et al.] // Sleep Breath. — 2012. — № 16. — P.1151—1158.
- Deurenberg, P. Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship / P. Deurenberg, M. Deurenberg-Yap, S. Guricci // Obes. Rev. — 2002. — № 3. — P.141—146.
- Kagawa, M. Body composition and anthropometry in Japanese and Australian Caucasian males and Japanese female / M. Kagawa, C.B. Binns, A.P. Hills // Asia Pac. J. Clin. Nutr. — 2007. — № 16 (1). — P.31—36.
- Cakirer, B. The relationship between craniofacial morphology and obstructive sleep apnea in whites and in African-Americans / B. Cakirer, M.G. Hans, G. Graham // Am. J. Respir. Crit. Care Med. — 2009. — № 163. — P.947—950.
- Lavie, P. Obstructive sleep apnea syndrome as a risk factor for hypertension: population study / P. Lavie, P. Herer, V. Hoffstein // BMJ. — 2000. — № 320. — P.479—482.
- Association of sleep-disordered breathing and the occurrence of stroke / M. Arzt, T. Young, L. Finn [et al.] // Am. J. Respir. Crit. Care Med. — 2005. — № 172. — P.1447—1451.
- Punjabi, N.M. Disorders of glucose metabolism in sleep apnea / N.M. Punjabi, V.Y. Polotsky // J. Appl. Physiol. — 2005. — № 99. — P.1998—2007.
- Vgontzas, A.N. Sleep apnoea is a manifestation of the metabolic syndrome / A.N. Vgontzas, E.O. Bixler, G.P. Chrousos // Sleep Med. Rev. — 2005. — № 9. — P.211—224.
- Owens, R.L. Upper airway function in the pathogenesis of obstructive sleep apnea: a review of the current literature / R.L. Owens, D.J. Eckert, S.Y. Yeh// Curr. Opin. Pulm. Med. — 2008. — № 14. — P.519—524.
- Lam, B. Obstructive sleep apnea in Asia / B. Lam, D.C. Lam, M.S. Ip // Int. J. Tuberc. Lung Dis. Respirology. — 2007. — № 11 (1). — P.2—11.
- Durrence, H.H. The sleep of African Americans: a comparative review / H.H. Durrence, K.L. Lichstein // Behav. Sleep. Med. — 2006. — № 4 (1). — P.29—44.
- Villaneuva, A.T. Ethnicity and obstructive sleep apnoea / A.T. Villaneuva, P.R. Buchanan, B.J. Yee // Sleep Med. Rev. — 2005. — № 9. — P.419—436.
- Gender differences in sleep apnea: the role of neck circumference / D.R. Dancey, P.J. Hanly, C. Soong [et al.] // Chest. — 2003. — № 123. — P.1544—1550.
- Ethnicity as a risk factor for obstructive sleep apnea: comparison of Japanese descendants and white males in Sаo Paulo, Brazil / P.R. Genta, B.F. Marcondes, N.J. Danzi [et al.] // Braz. J. Med. Res. Biol. — 2008. — № 41 (8). — P.728—733.
- Lam, B. Obstructive sleep apnea in Asia / B. Lam, D.C. Lam, M.S. Ip // Int. J. Tuberc. Lung. Dis. Respirology. — 2007. — № 11 (1). — P.2—11.
- Douglas, N.J. Home diagnosis of the obstructive sleep apnea/hypopnea syndrome / N.J. Douglas // Sleep Med. Rev. — 2003. — № 7. — P.53—59.
- Mehta, A. A randomized, controlled study of a mandibular advancement splint for obstructive sleep apnea / A. Mehta, J. Qian, P. Petocz [et al.] // Am. J. Respir. Crit. Care Med. — 2001. — № 163. — P.1457—1461.
- Obstructive Sleep Apnea: From pathogenesis to treatment: Current controversies and future directions/ P.R. Eastwood, A. Malhotra, L.J. Palmer [et al.] // Respirology. — 2010. — № 15. — P.587—595.
- Pack, A.I. Advances in sleep-disordered breathing / A.I. Pack // Am. J. Respir. Crit. Care Med. — 2006. — № 173. — P.7—15. 54.
- Johansson, K. Longer term effects of very low energy A.S. Chan, K. Sutherland, R.J. Schwab // Thorax. — diet on obstructive sleep apnea in cohort derived from 2010. — № 65. — P.726—732. randomised controlled trial: prospective observational 57. Lindman, R. A review of oral devices in the treatment follow-up study / K. Johansson, E. Hemmingsson, of habitual snoring and obstructive sleep apnoea / R.R. Harlid // BMJ. — 2011. — № 342. — P.3017. R. Lindman, L. Bondemark // Swed. Dent. J. — 2001. —
- Tachibana, N. Imbalance between the reality of sleep № 25. — P.39—51. specialists and the demands of society in Japan / 58. Sher, A.E. Upper airway surgery for obstructive sleep N. Tachibana // Ind. Health. — 2005. — № 43. — P.49— apnea / A.E. Sher // Sleep Med. — 2002. — № 6. — 52. P.195—212.
- Chan, A.S. The effect of mandibular advancement 59. Verse, T. Bariatric surgery for obstructive sleep apnea on upper airway structure in obstructive sleep apnea/ / T. Verse // Chest. — 2005. — № 128. — P.485—487.
 CARDIAC TUMORS IN CLINICAL PRACTICE
CARDIAC TUMORS IN CLINICAL PRACTICE
DOI: 10.20969/ VSKM.2017.10(4).80-86
MIKHOPAROVA OLGA Y., Head of the Department of functional diagnostic of Clinical hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan, Russia, 420059, Kazan, Orenburg tract str., 132, e-mail: olga-mihoparova@rambler.ru
TCYBULKIN NIKOLAY A., C. Med. Sci., associate professor of the Department of cardiology, roentgen-endovascular and cardiovascular surgery of Kazan State Medical Academy — of the branch of Russian Medical Academy of Postgraduate Education, Russia, 420012, Kazan, Butlerov str., 36, e-mail: kldkgma@mail.ru
OSHCHEPKOVA OLGA B., Head of the Department of cardiology of Clinical hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan, Russia, 420059, Kazan, Orenburg tract str., 132, e-mail: oschepkova.kazan@mail.ru
TUKHVATULLINA GALINA V., Head of Clinical diagnostic laboratory of Clinical Hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan, Russia, 420059, Kazan, Orenburg tract str., 132, e-mail: galatuhvatullina@mail.com ;
Abstract. Aim. Characteristics of current view on tumor lesions of heart in daily clinical practice of cardiologist are presented. Material and methods. Review of scientific medical literature on subject of tumor lesions of the heart. Results and discussion. Heart tumors are infrequent but they do represent essential diagnostic difficulties. Heart tumors are classified as primary and metastatic. The most frequent types of benign tumors are myxomas of auricles demonstrating exophytic growth, whereas sarcomas of invasive nature are considered the most malignant primary tumors. Primary malignant tumors in lungs and mediastinum are frequent reasons of metastatic tumor lesion of the heart, in particular the tumors of esophagus and lymphomas. The histological sectioning of the tumors on benign and malignant is essential but it does not always define the character of clinical course of the disease. The main diagnostic methods of heart tumors are echocardiography, magnetic resonance tomography and computer tomography scan. The final diagnosis of heart tumors is made according to the results of biopsy which is carried out by minimally traumatic accesses or by the means of mediastinoscopy or thoracotomy. Conclusion. Timely detection of heart tumors demands integrated diagnostic approach and interaction of doctors of various specialties such as clinical cardiologists, ultrasonic and radiographic diagnosticians, specialists in functional and laboratory diagnostics, histologists and cytologists.
Key words: cardiac tumors, classification, diagnosis, clinical development.
For reference: Mikhoparova OY, Tcybulkin NA, Oshchepkova OB, Tukhvatullina GV. Cardiac tumors in clinical practice. The Bulletin of Contemporary Clinical Medicine. 2017; 10 (4): 80—86. DOI: 10.20969/ VSKM.2017.10(4).80-86.
Refereneces
- Amirov NB ed. Ishemicheskaja bolezn’ serdca v obshhej vrachebnoj praktike: diagnostika, lechenie i profilaktika: monografija [Ischemic heart disease in general medical practice: diagnosis, treatment and prevention: monograph]. Kazan’: «Orange-k». 2011; 194 p.
- Davhale R, Potapova MV, Amirov NB. Rasprostranennost’ arterial’noj gipertenzii sredi sotrudnikov pravoohranitel’nyh organov (obzor literatury) [Prevalence of arterial hypertension among law enforcement officers (literature review)]. Vestnik sovremennoj klinicheskoj mediciny [The Bulletin of contemporary clinical medicine]. 2013; 6 (2): 66-73.
- Muhametshina GA, Amirov NB, Frolova JeB, Agliullina FF, Muhametzjanova NA, Morozova AA. Ostryj miokardit v praktike vracha (opisanie klinicheskogo sluchaja) [Acute myocarditis in the practice of a physician (description of a clinical case)]. Vestnik sovremennoj klinicheskoj mediciny [The Bulletin of contemporary clinical medicine]. 2013; 6 (4): 57-62.
- Sajfullina GB, Ahunova SJu, Sadykov AR, Ibatullin MM, Amirov NB. Konechno-diastolicheskij ob#em levogo zheludochka kak prognosticheskij pokazatel’ postoperativnogo remodelirovanija levogo zheludochka u pacientov s ishemicheskoj kardiomiopatiej: sravnitel’nye dannye jehokardiografii i perfuzionnoj tomoscintigrafii miokarda [Final diastolic volume of the left ventricle as a prognostic indicator of postoperative remodeling of the left ventricle in patients with ischemic cardiomyopathy: comparative data of echocardiography and perfusion tomoscintigraphy of the myocardium]. Materialy Rossijskogo nacional’nogo kongressa kardiologov «Innovacii i progress v kardiologii» [Materials of the Russian National Congress of Cardiology «Innovations and progress in cardiology»]. 2014; 414.
- Lestuzzi C. Primary tumors of the heart. Curr Opin Cardiol. 2016; 31 (6): 593-598.
- Styring E, Billing V, Hartman L, et al. Simple guidelines for efficient referral of soft-tissue sarcomas: a populationbased evaluation of adherence to guidelines and referral patterns. J Bone Joint Surg Am. 2012; 18: 94 (14): 12911296.
- Rice DC, Reardon MJ. Left heart sarcomas. Methodist Debakey Cardiovasc J. 2010; 6 (3): 49-56.
- Lestuzzi C, De Paoli A, Baresic T, et al. Malignant cardiac tumors: diagnosis and treatment. Future Cardiol. 2015; 11 (4): 485-500.
- Molina JE, Edwards JE, Ward HB. Primary cardiac tumors: experience at the University of Minnesota. Thorac Cardiovasc Surg. 1990; 38 (Suppl 2): 183-191.
- Nair A, Rajesh GN, Sajeev CG. Functional tricuspid stenosis: a rare presentation of suspected rhabdomyoma as congenital cyanotic heart disease. Cardiol Young. 2017; 12: 1-4.
- Djordjevic SA, Glumac S, Kalanj J. Cardiac haemangioma associated with a duct-dependent congenital heart disease in a newborn infant. Cardiol Young. 2017; 12: 1-3.
- Castillo JG, Silvay G. Characterization and management of cardiac tumors. Semin Cardiothorac Vasc Anesth. 2010; 14 (1): 6-20.
- Duquesne I, Sanchez-Salas R, Zannis K, et al. Concomitant Heart, Ovaries, and Renal Neoplasms: Atypical Findings During Hypertension Evaluation. Curr Urol Rep. 2016; 17 (12): 85.
- Jariwala P, Kale SS. CD20 negative B-cell lymphoma presenting as constrictive pericarditis: Rare etiology of acute heart failure. Indian Heart J. 2016; 68 (Suppl 2): 253-257.
- Arimoto J, Higurashi T, Kato S, et al. Cardiac tumors and gastroendoscopy: endoscopic resection of left ventricular tumors. Endoscopy. 2017; 49 (S 01): 23-24.
- Yuan S-M. Fetal Primary Cardiac Tumors During Perinatal Period. Pediatrics and Neonatology. 2016; http://dx.doi. org/10.1016/j.pedneo.2016.07.004
- Lüscher TF. Tumours and the heart: common risk factors, chemotherapy, and radiation. Eur Heart J. 2016; 21; 37 (36): 2737-2738.
- Blackmon SH, Reardon MJ. Pulmonary artery sarcoma. Methodist Debakey Cardiovasc J. 2010; 6 (3): 38-43.
- Mizia-Malarz A, Sobol-Milejska G, Buchwald J, Woś H. Inflammatory Myofibroblastic Tumor of the Heart in the Infant: Review of the Literature. J Pediatr Hematol Oncol. 2016; 38 (8): 298-302.
- Shi L, Wu L, Fang H, et al. Identification and clinical course of 166 pediatric cardiac tumors. Eur J Pediatr. 2017; 176 (2): 253-260.
- Vander Salm TJ. Unusual primary tumors of the heart. Semin Thorac Cardiovasc Surg. 2000; 12 (2): 89-100.
- Pontone G, Di Bella G, Silvia C, et al. Clinical recommendations of cardiac magnetic resonance, Part II: inflammatory and congenital heart disease, cardiomyopathies and cardiac tumors: a position paper of the working group ‘Applicazioni della Risonanza Magnetica’ of the Italian Society of Cardiology. J Cardiovasc Med (Hagerstown). 2017; 18 (4): 209-222.
- Giusca S, Mereles D, Ochs A, et al. Incremental value of cardiac magnetic resonance for the evaluation of cardiac tumors in adults: experience of a high volume tertiary cardiology centre. Int J Cardiovasc Imaging. 2017; 30: doi: 10.1007/s10554-017-1065-7.
- Taegtmeyer H, Karlstaedt A, Rees ML, Davogustto G. Oncometabolic Tracks in the Heart. Circ Res. 2017; 20; 120 (2): 267-269.
- Sarjeant JM, Butany J, Cusimano RJ. Cancer of the heart: epidemiology and management of primary tumors and metastases. Am J Cardiovasc Drugs. 2003; 3 (6): 407-421.
- Reardon MJ, Walkes JC, Benjamin R. Therapy insight: malignant primary cardiac tumors. Nat Clin Pract Cardiovasc Med. 2006; 3 (10): 548-553.
- Elbardissi AW, Dearani JA, Daly RC, et al. Survival after resection of primary cardiac tumors: a 48-year experience. Circulation. 2008; 30; 118 (14 Suppl): 7-15.
 ORGANIZATION OF PUBLIC CONTRACTING ON MEDICAL SERVICE PROVISION TO EMPLOYEES OF INTERNAL AFFAIRS BODIES AT THE MEDICAL UNIT OF THE MINISTRY OF INTERNAL AFFAIRS OF RUSSIA IN THE REPUBLIC OF TATARSTAN
ORGANIZATION OF PUBLIC CONTRACTING ON MEDICAL SERVICE PROVISION TO EMPLOYEES OF INTERNAL AFFAIRS BODIES AT THE MEDICAL UNIT OF THE MINISTRY OF INTERNAL AFFAIRS OF RUSSIA IN THE REPUBLIC OF TATARSTAN
UDC 614.21:351.74(470.41):616-057.36-082
DOI: 10.20969/VSKM.2017.10(4).87-91
GAZIMOVA LILIYA G., Head of the Department of medical service performance evaluation, organizational methodological and preventative therapeutic unit of the Medical Unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan, Russia, 420101, Kazan, Lobachevsky str., 13, e-mail: lilya2603@mail.ru ;
Abstract. In case of the absence of medical organizations or particular departments or, as a rule, special medical equipment, at the station, at the place of residence or other location, employees of the Ministry of Internal Affairs of the Russian Federation have a right on emergency medical care in medical organizations of state and municipal Healthcare system of the Russian Federation, according to the indications. Aim. Analysis of public contracting organization on rendering medical services for the employees of Internal Affairs bodies for 2012-2016, has been performed. Material and methods. The analysis of activities has been carried out for the five-year period according to annual reports applying the methods of statistical processing. The legal framework of public contracts on medical service provision has been reflected. Results and discussion. The paper summarizes five years of experience in providing medical service in medical organizations of the public healthcare system. The problematic issues are being considered. Conclusion. Public contracting on medical service provision to internal affairs bodies’ officers is effective. It allows them to receive the full amount of medical care efficiently and in a timely manner.
Key words: public contract on medical service provision for the employees of internal affairs bodies, medical care, legal bases of the medical service provision organization.
For reference: Gazimova LG. Organization of public contracting on medical service provision to employees of internal affairs bodies at the medical unit of the Ministry of internal affairs of Russia in the Republic of Tatarstan. The Bulletin of Contemporary Clinical Medicine. 2017; 10 (4): 87—91. DOI: 10.20969/ VSKM.2017.10(4).87-91.
Refereneces
- Federal’nyj zakon ot 30/11/2011 goda № 342-FZ «O sluzhbe v organah vnutrennih del Rossijskoj Federacii i vnesenii izmenenij v otdel’nye zakonodatel’nye akty Rossijskoj Federacii» [The Federal law from 30/11/2011 № 342-FZ «On service in bodies of internal Affairs of the Russian Federation and amendments to certain legislative acts of the Russian Federation»].
- Federal’nyj zakon ot 07/02/2011 goda № 3-FZ «O policii» [Federal law of 07/02/2011 № 3-FZ «On police»].
- Federal’nyj zakon ot 19/07/2011 goda № 247-FZ «O social’nyh garantijah sotrudnikam organov vnutrennih del Rossijskoj Federacii i vnesenii izmenenij v otdel’nye zakonodatel’nye akty Rossijskoj Federacii» [Federal law of 19/07/2011 № 247-FZ «About social guarantees to employees of internal Affairs bodies of the Russian Federation and amendments to certain legislative acts of the Russian Federation»].
- Federal’nyj zakon ot 05/04/2013 goda № 44-FZ «O kontraktnoj sisteme v sfere zakupok tovarov, rabot, uslug dlja obespechenija gosudarstvennyh i municipal’nyh nuzhd» [Federal law of 05/04/2013 № 44-FZ «On contract system in procurement of goods, works, services for state and municipal needs»].
- Postanovlenie Pravitel’stva Rossijskoj Federacii ot 30/12/2011 № 1232 «O porjadke okazanija sotrudnikam organov vnutrennih del Rossijskoj Federacii, otdel’nym kategorijam grazhdan Rossijskoj Federacii, uvolennyh so sluzhby v organah vnutrennih del, i chlenam ih semej medicinskoj pomoshhi i ih sanatorno-kurortnogo obespechenija» [Resolution of the Government of the Russian Federation of 30/12/2011 № 1232 «On the procedure of providing officers of the internal Affairs of the Russian Federation separate categories of citizens of the Russian Federation dismissed from service in bodies of internal Affairs, and members of their families medical care and sanatorium-resort services»].
- Prikaz MVD Rossii ot 08/11/2006 goda № 895 «Ob utverzhdenii Polozhenija ob organizacii medicinskogo obsluzhivanija i sanatorno-kurortnogo lechenija v medicinskih uchrezhdenijah sistemy MVD Rossii» [The Ministry of internal Affairs order dated 08/11/2006, № 895 «On approval of regulations on the organization of medical care and sanatorium treatment in medical institutions of Ministry of internal Affairs of Russia»].
-
7. Galiullin AD, Potapova MV, Gasimova LG. Otdelenie kachestva okazanija medicinskoj pomoshhi MSCh MVD PO RT i ego dejatel’nost’ v 2007-2008 gg [Medical aid quality expertise department of the Medical sanitary department of the ministry of internal affairs on RT and its activity in 2007-2008]. Vestnik sovremennoj klinicheskoj mediciny [The Bulletin of Contemporary Clinical Medicine]. 2008; 1 (1): 136-137.
 RESULTS OF QUALITY MANAGEMENT SYSTEM SELF-EVALUATION IN A MULTI-SPECIALTY HOSPITAL
RESULTS OF QUALITY MANAGEMENT SYSTEM SELF-EVALUATION IN A MULTI-SPECIALTY HOSPITAL
UDC 614.21:351.74(470.41):005.6
DOI: 10.20969/ VSKM.2017.10(4).91-95
SABIROV LENAR F., C. Med. Sci., Head of Clinical hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan, Russia, 420059, Kazan, Orenburg tract str., 132; associate professor of the Department of public health, economics and health management of Kazan State Medical Academy — the branch of Russian Medical Academy of Postgraduate Education, Russia, 420012, Kazan, Butlerov str., 36, tel. 8(843)277-88-84, e-mail: hospital_kaz16@mvd.ru ;
Abstract. Aim. Analysis of the quality management system effectiveness at Clinical Hospital of medical unit of the Russian Ministry of Internal Affairs in the Republic of Tatarstan has been carried out through self-assessment of the current quality management system. The level of readiness of the quality management system has been determined. Material and methods. According to the results of the survey of process owners and the heads of departments of the Clinical Hospital of medical unit of the Russian Ministry of Internal Affairs in the Republic of Tatarstan using the questions on initial self-assessment, quality management principles that have to be improved have been identified. Priority directions of action to be used for event planning have been specified with their subsequent execution and control. Results and discussion. Hospital quality management system based on the principles of system and process approach to organization of medical care is effectively functioning. Regulatory framework supporting the structure of the quality management system allowing planning, implementation and constant monitoring of the activities on improvement of organization function, has been created. Criteria of quality management system process performance and the main directions of personnel management have been determined. Moreover, organizational chart for analysis by the hospital managers, allowing timely responding to the changes in macro and micro environment and evaluating decision effectiveness in the field of quality management, has been developed. Conclusion. Self-assessment of the quality management system of Clinical Hospital of medical unit of the Russian Ministry of Internal Affairs in the Republic of Tatarstan has showed a high level of readiness. Identification of priority directions of action to be applied for event planning, their subsequent execution and control, has appeared as a result of self-evaluation.
Key words: management, quality, health, self-evaluation.
For reference: Sabirov LF. Results of quality management system self-evaluation in a multi-specialty hospital. The Bulletin of Contemporary Clinical Medicine. 2017; 10 (4): 91—95. DOI: 10.20969/ VSKM.2017.10(4).91-95.
Refereneces
- Brjuhanova NG. Reformirovanie vedomstvennogo zdravoohranenija: opyt i perspektivy [The reform of the institutional health care: the experience and prospects]. Bjulleten’ Nacional’nogo nauchno-issledovatel’skogo instituta obshhestvennogo zdorov’ja imeni NA Semashko [Bulletin of the National research Institute of public health named after NA Semashko]. 2005; 2: 105–107.
- Ukaz Prezidenta Rossijskoj Federacii ot 31 dekabrja 2015 goda No 683 «O strategii nacional’noj bezopasnosti Rossijskoj Federacii» [The decree of the President of the Russian Federation from December, 31st, 2015 No 683 «On the strategy of national security of the Russian Federation»].
- Volkov AI, Polesskij VA, Martynchik SA. Kljuchevye strategii VOZ po sovershenstvovaniju nacional’nyh sistem zdravoohranenija [Key strategies by the who to improve national health systems]. Glavvrach [Doctor]. 2008; 5: 10–25.
- Sabirov LF, Spiridonov AV. Opyt vnedrenija sistemy menedzhmenta kachestva ISO 9001-2008 v klinicheskom gospitale MSCh MVD Rossii po Respublike Tatarstan [The experience of implementation of quality management system ISO 9001-2008 in clinical hospital of MSU of the Ministry of internal Affairs of Russia in Republic of Tatarstan]. Vestnik sovremennoj klinicheskoj mediciny [Bulletin of contemporary clinical medicine]. 2011; 4 (4): 35–38.
- Galeev VI. Samoocenka dejatel’nosti organizacii na sootvetstvie kriteriem premii Pravitel’stva RF v oblasti kachestva 2009 godu: rekomendacii [Self-assessment of the organization’s activities for compliance with the criteria of the RF Government prize in the eld of quality 2009: recommendations]. Moskva [Moscow]: «VNIIS». 2009; 78 p.
- Konti T. Samoocenka v organizacijah [Self-assessment in organizations]/ Moskva: RIA «Standarty i kachestvo» [Moscow: RIA «Standards and quality»]. 2002; 327 p.
 ORGANIZATION AND THE WAYS OF HOSPITAL CARE REFINEMENT TO EMPLOYEES OF THE MINISTRY OF INTERNAL AFFAIRS IN OF THE REPUBLIC BASHKORTOSTAN IN THE HOSPITAL OF THE MINISTRY OF INTERNAL AFFAIRS OF RUSSIA IN THE REPUBLIC OF BASHKORTOSTAN
ORGANIZATION AND THE WAYS OF HOSPITAL CARE REFINEMENT TO EMPLOYEES OF THE MINISTRY OF INTERNAL AFFAIRS IN OF THE REPUBLIC BASHKORTOSTAN IN THE HOSPITAL OF THE MINISTRY OF INTERNAL AFFAIRS OF RUSSIA IN THE REPUBLIC OF BASHKORTOSTAN
UDC 614.21:351.74(470.57):616-082-039.72
DOI: 10.20969/VSKM.2017.10(4).95-101
FAYZULLIN ILGIZ F., deputy Head of the Department of medical and preventive of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Republic of Bashkortostan, Russia, 450000, Ufa, K. Marx str., 59, tel. 8-347-279-44-47, e-mail: uriruss@mail.ru
GIZATULLIN TAGIR R., C. Med. Sci., associate professor of the Department of public health and health management of Institute of Public Health of Bashkir State Medical University, Russia, 450000, Ufa, Lenin str., 3
AKHMEROVA SVETLANA H., D. Med. Sci., professor of the Department of public health and health management of Institute of Public Health of Bashkir State Medical University, Russia, 450000, Ufa, Lenin str., 3
Abstract. Aim. The ways of medical care refinement to employees of internal affairs bodies on the basis of the hospital of Medical Unit of the Ministry of Internal Affairs of Russia in the Republic of Bashkortostan have been justified. Material and methods. Analysis of medical care provision to employees of the Ministry of Internal Affairs in Bashkortostan Republic in the hospital of medical unit of the Ministry of Internal Affairs in the Republic of Bashkortostan, for 10 years (since 2007 till 2016) has been performed. Runtime reports on activities of the hospital of Medical Unit of the Ministry of Internal Affairs of Russia in the Republic of Bashkortostan for the period from 2007 to 2016, such as 4-MED, 5-ZAB, 6-VUT forms (approved by the order of the Ministry of Internal Affairs of Russia from 07.10.2015 № 962 «On the system of organization of statistical reporting in medical organizations of the system of the Ministry of Internal Affairs of the Russian Federation») and the database of the program «Statistics of the Medical unit», have been used as the sources. Results and discussion. Proposals have been made in order to optimize the work of the hospital, improve the quality and accessibility of medical care and to reduce the costs on treatment for the personnel of the Ministry of Internal Affairs in the Republic of Bashkortostan in healthcare facilities of the Ministry of Health in Bashkortostan. Conclusion. Expanding the range of provided medical services and opening the most demanded departments equipped with all necessary machines is aimed at reducing the cost of medical care in third-party medical organizations and increasing the volume and quality of medical care provided to employees of internal affairs bodies in the hospital of the Ministry of Internal Affairs of Russia in the Republic of Bashkortostan.
Key words: employees of law-enforcement bodies, medical support, Medical Care unit of the Ministry of Internal Affairs of Russia in the Republic of Bashkortostan.
For reference: Fayzullin IF, Gizatullin ТR, Akhmerova SG. Organization and the ways of hospital care refinement to employees of the Ministry of Internal Affairs in Bashkortostan Republic in the hospital of the Ministry of Internal Affairs of Russia in the Republic of Bashkortostan. The Bulletin of Contemporary Clinical Medicine. 2017; 10 (4): 95—101. DOI: 10.20969/ VSKM.2017.10(4).95-101.
Refereneces
- Yudaeva KV, Yasin EG. Strategija 2050: spravitsja li Rossija s vyzovami globalizacii? [Strategy 2050: will Russia cope with the challenges of globalization?]. Voprosy jekonomiki [Issues of economics]. 2008; 5: 4-21.
- Kleeva LP, Vorobiev IV. Ocenka urovnja innovacionnogo razvitija otechestvennoj jekonomiki [An estimation of a level of innovative development of a domestic economy]. Kreativnaja jekonomika [The Creative economy]. 2011; 9 (57): 98-107.
- Kirichek EV. Social’naa i pravovaja zashhishhennost’ sotrudnikov organov vnutrennih del v sovremennoj Rossii [Social and legal protection of employees of law enforcement bodies in modern Russia]. Juridicheskaja nauka i pravoohranitel’naja praktika [Juridical science and law enforcement practice]. 2010; 4 (14): 21-30.
- Shakalov II. Imidzh rossijskih organov vnutrennih del v 2012 godu: predvaritel’nye itogi reformy (po rezul’tatam kompleksnogo izuchenija obshhestvennogo mnenija) [The image of the Russian Interior Ministry in 2012: preliminary results of the reform (based on the results of a comprehensive study of public opinion)]. Vestnik Adygejskogo Gosudarstvennogo Universiteta [Bulletin of the Adyghe State University]. 2012; 3 (105): 2.
- Sidorenko VA. Vedomstvennoe zdravoohranenie: istorija, sostojanie, perspektivy [Departmental health care: history, condition, prospects]. Medicinskij vestnik MVD [Medical Bulletin of the Ministry of Internal Affairs]. 2016; 6: 2-9.
- Evkhuta DV, Lishakov VB. O sovershenstvovanii struktury medicinskoj sluzhby Vooruzhennyh Sil [On the improvement of the structure of the medical service of the Armed Forces]. Voennaja medicina [Military medicine]. 2013; 2: 2-7.
- Khisamiyev RSh, Ginjatullina LR, Amirov NB. Dostizhenija i perspektivy razvitija vedomstvennoj medicinskoj sluzhby MVD po Respublike Tatarstan [Departmental health care of ministry of the interior in the Tatarstan Repablic: Reality and perspectives]. Vestnik sovremennoj klinicheskoj mediciny [The Bulletin of Contemporary Clinical Medicine]. 2016; 9 (6): 13-15.
- Evkhuta DV, Lishakov VB, Strinkevich AL. O povyshenii jeffektivnosti dejatel’nosti medicinskoj sluzhby Vooruzhennyh Sil i optimizacii organizacionno-shtatnoj struktury voennyh medicinskih organizacij i podrazdelenij [On increasing the effectiveness of the medical service of the Armed Forces and optimizing the organizational structure of military medical organizations and units]. Voennaja medicina [Military medicine]. 2014; 1: 2-7.
- Surmievich PE. Nauchnoe obosnovanie sistemy medicinskih profilakticheskih meroprijatij sredi sotrudnikov organov vnutrennih del [Scientific substantiation of the system of medical preventive measures among employees of lawenforcement bodies]. SPb [St Petersburg]. 2003; 176 p.
- Dyakovich MP, Bush MP. Rannie klinicheskie izmenenija i jemocional’noe vygoranie u sotrudnikov policii [Early clinical changes and emotional burnout of police officers]. Medicina truda i promyshlennaja jekologija [Occupational medicine and industrial ecology]. 2015; 12: 37-41.
- Dyakovich MP, Pavlov AV. Mediko-psihologicheskie i social’nye aspekty professional’noj adaptacii sotrudnikov ugolovno-ispolnitel’noj sistemy [Medico-psychological and social aspects of professional adaptation of the staff of the penitentiary system]. Voenno-medicinskij zhurnal [Military Medical Journal]. 2010; 2: 42-46.
- Davhale R, Potapova MV, Amirov NB. Rasprostranennost’ arterial’noj gipertenzii sredi sotrudnikov pravoohranitel’nyh organov (obzor literatury) [Prevalence of hypertension among law enforcement bodies (literature review)]. Vestnik sovremennoj klinicheskoj mediciny [The Bulletin of contemporary clinical medicine]. 2013; 6 (2): 66– 72.
- Postanovlenie Pravitel’stva Rossijskoj Federacii ot 30/12/2011 goda № 1232 «O porjadke okazanija sotrudnikam organov vnutrennih del Rossijskoj Federacii, otdel’nym kategorijam grazhdan Rossijskoj Federacii, uvolennyh so sluzhby v organah vnutrennih del, i chlenam ih semej medicinskoj pomoshhi i ih sanatorno-kurortnogo obespechenija» [Decree of the Government of the Russian Federation of 30/12/2011 #1232 «On the procedure for rendering medical aid and sanatorium-and-spa provision to employees of the internal affairs bodies of the Russian Federation, certain categories of citizens of the Russian Federation, dismissed from the service in internal affairs bodies, and members of their families»].
- Sovmestnyj prikaz Ministerstva vnutrennih del i Ministerstva zdravoohranenija Respubliki Bashkortostan ot 14/02/2012 goda № 114/314-D «Ob okazanii medicinskoj pomoshhi sotrudnikam organov vnutrennih del Rossijskoj Federacii v uchrezhdenijah gosudarstvennoj ili municipal’noj sistemy zdravoohranenija Respubliki Bashkortostan» [Joint Order of the Ministry of Internal Affairs and the Ministry of Health of the Republic of Bashkortostan of 14/02/2012 № 114/314-D «On rendering medical assistance to employees of the internal affairs of the Russian Federation in institutions of the state or municipal health system of the Republic of Bashkortostan»].
 50 YEARS OF THE DEPARTMENT OF TRAUMATOLOGY, ORTHOPEDICS AND EXTREME CONDITION SURGERY OF KAZAN STATE MEDICAL UNIVERSITY
50 YEARS OF THE DEPARTMENT OF TRAUMATOLOGY, ORTHOPEDICS AND EXTREME CONDITION SURGERY OF KAZAN STATE MEDICAL UNIVERSITY
UDC (616-001+617.3):378.661(470.41-25).096(091)
DOI: 10.20969/ VSKM.2017.10(4).102-104
CHIKAEV VYACHESLAV F., D. Med. Sci, professor of the Department of traumatology, orthopedics and extreme condition surgery of Kazan State Medical University, Russia, 420012, Kazan, Butlerov str., 49, e-mail: prof.chikaev@gmail.com
FAIZRAKHMANOVA GULNARA M., C. Med. Sci., assistant of professor of the Department of traumatology, orthopedics and extreme condition surgery of Kazan State Medical University, Russia, 420012, Kazan, Butlerov str., 49, e-mail: fagumu69@mail.ru
EMELIN ALEXEY L., C. Med. Sci., assistant of professor of the Department of traumatology, orthopedics and extreme condition surgery of Kazan State Medical University, Russia, 420012, Kazan, Butlerov str., 49, e-mail: Travmatica@mail.ru ;
Abstract. In 2017 department of traumatology, orthopedics and extreme condition surgery at Kazan State Medical University turns 50 years old. Aim. Historical development of Department of Traumatology, Orthopedics and Extreme Condition Surgery has been studied. Material and methods. The stages of development of the department as well as the results of scientific and practical research are shown according to archival material. Results and discussion. Department founded in 1967 initially united 3 specialties: traumatology-orthopedics, military surgery and neurosurgery. It was called Department of traumatology, orthopedics, and military surgery with the course of neurosurgery. The new Department was headed by doctor of medical science, Professor Nikolaev Herman M. Since 1984 associate professor and later since 1988 professor Zulkarneev Renat A. was elected as the head of the Department. From 1997 to 1999 professor Dobrokvashin Sergey V. has been the interim Head of the Department. Later he was elected as the Head of Department of General surgery at Kazan State Medical University. Since 1999 the Department is headed by doctor of medical sciences Akhtyamov Ildar F. Conclusion. The research at the Department for today covers a variety of topics: major joint endoprosthesis replacement, the problem of thromboembolic complication prevention in surgery, diagnosis and treatment of multiple associated injuries, chest and abdomen trauma and their complications.
Key words: department, traumatology, orthopedics, history.
For reference: Chikaev VF, Faizrakhmanova GM, Emelin AL. 50 years of the Department of traumatology, orthopedics and extreme condition surgery of Kazan State Medical University. The Bulletin of Contemporary Clinical Medicine. 2017; 10 (4): 102—104. DOI: 10.20969/ VSKM.2017.10(4).102-104.
 PARANEOPLASTIC MENINGOENCEPHALITIS ASSOCIATED WITH B-CELL LYMPHOMA (clinical observation)
PARANEOPLASTIC MENINGOENCEPHALITIS ASSOCIATED WITH B-CELL LYMPHOMA (clinical observation)
UDC 616.831.9-002-02:616-006.441
DOI: 10.20969/ VSKM.2017.10(4).105-112
ZAKIROVA DILYARA R., Head of the Department of neurology of Clinical hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan, Russia, 420059, Kazan, Orenburgskiy tract str., 132, e-mail: dilyara.zakirova555@yandex.ru
IKSANOVA EKATERINA N., physician of the Department of neurology of Clinical hospital of the Medical Care unit of the Ministry of Internal of Russia Affairs in the Republic of Tatarstan, Russia, 420059, Kazan, Orenburgskiy tract str., 132, е-mail: iksanova_en@mail.ru
NABIULLINA GUZEL N., neurologist of the Department of neurology of Clinical hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan, Russia, 420059, Kazan, Orenburgskiy tract str., 132, е-mail: nabiullina96@yandex.ru
AMIROV NAIL B., D. Med. Sci, professor of the Department of general medical practice of Kazan State Medical University, Russia, 420012, Kazan, Butlerov str., 49, e-mail: namirov@mail.ru
KHUZINA GULNARA R., C. Med. Sci., associate professor of the Department of neurology and rehabilitation of Kazan State Medical University, Russia, 420012, Kazan, Butlerov str., 49, e-mail: gkhuzina@yandex.ru
Abstract. Aim. Evaluation of management of patient with paraneoplastic syndrome associated with B-cell lymphoma has been performed. The features of clinical manifestations have been presented on example of personal clinical observations. Differential diagnosis of meningoencephalitis has been described. Clinical efficiency of treatment, its tolerability and prognostic factors have been evaluated. Material and methods. Rare clinical case of patient A., 68 years old, diagnosed with paraneoplastic syndrome in a form of subacute paraneoplastic meningoencephalitis developed 2 years after the onset of b-cell lymphoma in the setting of anticancer therapy, is presented. The study includes the data from clinical, instrumental, laboratory examinations and neuroimaging. Results and discussion. Presented clinical observation has allowed to identify the features of clinical course of subacute paraneoplastic encephalitis as one of the most frequent variants of paraneoplastic syndrome as well as to determine some of the «trigger» criteria of the diagnostic algorithm for this disease. In particular, such criteria are: age range of the patients 55—70 years; acute- and subacute progressive cerebral neurological symptoms; higher cortical function disorders (progressive personality changes, emotional disorders, gross disturbance of memory and thinking), disturbances of consciousness (agitation, confusion, coma disorders); psychic disorders; epileptic seizures; the history of oncological awareness or previously diagnosed cancer, ruling out the signs of infectious or infectious-allergic origin of the inflammation according to immunological and neuroimaging methods. Conclusion. Timely diagnosis of paraneoplastic syndromes is highly relevant in neurological practice. It determines potential for survival for the patient.
Key words: paraneoplastic meningoencephalitis, b-cell lymphoma, magnetic resonance imaging, paraneoplastic syndrome.
For reference: Zakirova DR, Iksanova EN, Nabiullina GN, Amirov NB, Khuzina GR. Paraneoplastic meningoencephalitis associated with B-cell lymphoma: clinical observation. The Bulletin of Contemporary Clinical Medicine. 2017; 10 (4): 105—112. DOI: 10.20969/ VSKM.2017.10(4).105-112.
Refereneces
- Yakhno NN, Loshkina AB, Koberskaya NN, Makhitaryan EA, Zakharov VV. Dementsiya: rukovodstvo dlya vrachey [Dementia: a guide for physicians]. Moskva [Moscow]: MedPress — inform. 2011; 3: 272 p.
- Rees JH. Paraneoplastic syndromes: when to suspect, how to confirm, and how to manage. J Neurol Neurosurg Psychiatr. 2004; 75 (Suppl 2): 43-50.
- Damulin IV. Degenerativnyye zabolevaniya s kognitivnymi rasstroystvami; Bolezni nervnoy sistemy — pod redakciej Jahno NN, Shtul’man DR [Degenerative diseases, cognitive disorders; Diseases of the nervous system — Jahno NN, Shtul’man DR ed]. Moskva: Meditsina [Moscow: Medicine]. 2003; 2: 189–207.
- Darnell RB, Posner JB. Paraneoplastic syndromes affecting the nervous system. Semin Oncol. 2006; 33 (3): 270–98.
- Yesavage JA, O’Harra R, Kraemer H, et al. Modeling the prevalence and incidence of Alzheimer’s disease and mild cognitive impairment. J Psychiatr Res. 2002; 36: 281–286.
- Levin OS, Shtul’man DR. Nevrologiya: spravochnik prakticheskogo vracha [Neuroscience: a Handbook of a practical physician]. Moskva [Moscow]: MedPress-Inform, 2016; 10: 1024 p.
- Shancle WR, Romney AK, Hara J, et al. Methods to improve the detection of mild cognitive impairment. Proc Nat Ac Sci. 2005; 102 (13): 4919–4929.
 DIAGNOSIS OF IRRITABLE BOWEL SYNDROME (clinical case)
DIAGNOSIS OF IRRITABLE BOWEL SYNDROME (clinical case)
DOI: 10.20969/ VSKM.2017.10(4).113-120
SAFARGALIYEVA LILYA H., Head of the Department of internal medicine of Clinical hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan, Russia, 420059, Kazan, Orenburg tract str., 132, e-mail: Safargalieva.lilia@mail.ru
YAGFAROVA RITA R., physician of the Department of internal medicine of Clinical hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan, Russia, 420059, Kazan, Orenburg tract str., 132
SHARIPOVA ROZALIA R., physician of the Department of internal medicine of Clinical hospital of the Medical Care unit of the Ministry of Internal Affairs of Russia in the Republic of Tatarstan, Russia, 420059, Kazan, Orenburg tract str., 132, e-mail: sharipova.7@mail.ru
AMIROV NAIL B., D. Med. Sci., academician of Russian Academy of Natural Science, professor of the Department of general medical practice of Kazan State Medical University, Russia, 420012, Kazan, Butlerov str., 49, e-mail: namirov@mail.ru ;
Abstract. Aim. Review of the latest data on pathogenesis and diagnosis of irritable bowel syndrome has been performed with presentation of personal clinical example. Material and methods. The following keywords have been used to select relevant articles in e-library and MedLine databases: «irritable bowel syndrome», «diagnostics», «pathogenesis», «differential diagnostics». Medical history of the patient with irritable bowel syndrome has been analyzed. Results and discussion. Nowadays, genetic bases of the pathophysiology of irritable bowel syndrome as well as the interaction of endocrine cells of the gastrointestinal tract and enteric nervous system are being actively studied. Intestinal microbiome is being explored. Currently, the «gold» diagnostic standard is the Rome criteria, the IV revision of which was presented in May, 2016. Despite significant achievements in fundamental, clinical and epidemiological studies, the mechanisms of functional intestinal disorders development have not been fully studied and the newest version of Rome criteria allows diagnosing irritable bowel syndrome only clinically by excluding other diseases. In the presented clinical case diagnosis was made only after repeated consultations of different specialists, multiple diagnostic tests, by excluding more serious diseases. Conclusion. Despite the greatest prevalence of irritable bowel syndrome among all functional disorders, its diagnosis is associated with a substantial burden in healthcare resources.
Key words: irritable bowel syndrome, Rome IV diagnostic criteria, differential diagnosis.
For reference: Safargaliyeva LH, Yagfarova RR, Sharipova RR, Amirov NB. Diagnosis of Irritable Bowel Syndrome (clinical case). The Bulletin of Contemporary Clinical Medicine. 2017; 10 (4): 113—120. DOI: 10.20969/ VSKM.2017.10(4).113-120.
Refereneces
- Enck P, Aziz Q, Barbara G et al. Irritable bowel syndrome. Nat Rev Dis Primers. 2016; 24 (2): 16014.
- Longstreth GF, Thompson WG, Chey WD et al. Functional bowel disorders. Gastroenterology. 2006; 130: 1480–1491.
- Yakovenko AV, Ivanov AN, Pryanishnikova AS et al. Patogeneticheskiye podkhody v lechenii sindroma razdrazhennogo kishechnika [Pathogenetic approaches in the treatment of irritable bowel syndrome]. Lechashchiy vrach [The attending physician]. 2011; 7: 36–41.
- Yakovenko EP, Agafonova NA, Yakovenko AV et al. Rol’ motornykh narusheniy v mekhaizmakh razvitiya klinicheskikh proyavleniy sindroma razdrazhennogo kishechnika (SRK) i SRK–podobnykh narusheniy: voprosy terapii [The role of motor disorders in the mechanisms of the development of clinical manifestations of irritable bowel syndrome (IBS) and IBS–like disorders: questions of therapy]. Consilium medicum. 2011; 1: 69–73.
- Pogromov AP, Mnatsakanyan MG, Tashchyan OV. Rasprostranennost’ sindroma razdrazhennogo kishechnika [Prevalence of irritable bowel syndrome]. Klinicheskaya Meditsina [Clinical Medicine]. 2016; 94 (11): 869–874.
- Henström M, D’Amato M. Genetics of irritable bowel syndrome. Molecular and Cellular Pediatrics. 2016; 3: 7–12.
- El–Salhy M, Gundersen D, Gilja OH et al. Is irritable bowel syndrome an organic disorder? World J Gastroenterol. 2014; 20 (2): 384–400.
- Ostertag D, Annahazi A, Krueger D. Tryptase potentiates enteric nerve activation by histamine and serotonin: Relevance for the effects of mucosal biopsy supernatants from irritable bowel syndrome patients. Neurogastroenterol Motil. 2017; 3: 13070.
- Sidhu M, van der Poorten D. The gut microbiome. Aust Fam Physician. 2017; 46 (4): 206–211.
- Drossman DA, Hasler WL. Rome IV–functional GI disorders: disorders of gut–brain interaction. Gastroenterology. 2016; 150 (6): 1257–1261.
- Schmulson MJ, Drossman DA. What Is New in Rome IV. J Neurogastroenterol Motil. 2017; 23 (2): 151–163.
- Simren M, Palsson OS, Whitehead WE. Update on Rome IV Criteria for Colorectal Disorders: Implications for Clinical Practice. Curr Gastroenterol Rep. 2017; 19: 15-26.
- Ivashkin VT, Mayev IV, Sheptulin AA et al. Klinicheskiye rekomendatsii Rossiyskoy gastroenterologicheskoy assotsiatsii po diagnostike i lecheniyu funktsional’noy dispepsii [Clinical recommendations of the Russian Gastroenterological Association for the diagnosis and treatment of functional dyspepsia]. Rossiyskiy zhurnal gastroenterologii, gepatologii, koloproktologii [Russian Journal of Gastroenterology, Hepatology, Coloproctology]. 2017; 27 (1): 50–61.
- Padhy SK, Mishra S, Sarkar S et al. Comparison of psychiatric morbidity in patients with irritable bowel syndrome and non–ulcer dyspepsia. Ind Psychiatry J. 2016; 25 (1): 29–34.
- Buono JL, Carson RT, Flores NM. Health–related quality of life, work productivity, and indirect costs among patients with irritable bowel syndrome with diarrhea. Health Qual Life Outcomes. 2017; 15 (1): 35-42.
- Shklyayev AYe, Gorbunov YuV. Primeneniye spetsificheskogo i nespetsificheskogo oprosnikov dlya otsenki kachestva zhizni patsiyentov s funktsional’noy patologiyey kishechnika [Application of a specific and nonspecific questionnaire for assessing the quality of life of patients with functional bowel disease]. Arkhiv» vnutrenney meditsiny [Archive of Internal Medicine]. 2016; 30 (4): 53–57.
- Spiridonov AV, Absalyamova LR, Gimaletdinova IA. Sindrom razdrazhennogo kishechnika v praktike vracha–gastrojenterologa: ot mehanizmov vozniknovenija do jeffektivnoj terapii [Syndrome of the angry intestines in practice of the gastroenterologist: from emergence mechanisms before effective therapy]. Vestnik sovremennoj klinicheskoj mediciny [Bulletin of Contemporary Clinical Medicine]. 2015; 8 (6): 79–84.
- Spiridonov AV, Absaljamova LR, Gimaletdinova IA. Primenenie kratkogo oprosnika VOZ WHOQOL–BREF dlja ocenki kachestva zhizni pacientov s sindromom razdrazhennogo kishechnika [Appliance of the short questionnaire of WHOQOL–BREF by the WHO for quality of life assessment in irritable bowel syndrome patients]. Vestnik sovremennoj klinicheskoj mediciny [The Bulletin of Contemporary Clinical Medicine]. 2016; 9 (6): 76–81.
- Ivashkin VT, Poluektova YeA. Sindrom razdrazhennogo kishechnika: patofiziologicheskiye i klinicheskiye aspekty problemy [Irritable bowel syndrome: pathophysiological and clinical aspects of the problem]. Rossiyskiy zhurnal gastroenterologii, gepatologii, koloproktologii [Russian Journal of Gastroenterology, Hepatology, Coloproctology]. 2015; 25 (1): 4–16.
- Shul’pekova YuO, Baranskaya YeK. Differentsial’naya diagnostika sindroma razdrazhennogo kishechnika i glyutenovoy enteropatii [Differential diagnosis of irritable bowel syndrome and gluten enteropathy]. Rossiyskiy zhurnal Gastroenterologii, Gepatologii, Koloproktologii [Russian Journal of Gastroenterology, Hepatology, Coloproctology]. 2009; 6: 39– 48.
- Buono JL, Mathur K, Averitt AJ, Andrae DA. Economic Burden of Irritable Bowel Syndrome with Diarrhea: Retrospective Analysis of a US Commercially Insured Population. J Manag Care Spec Pharm. 2017; 23 (4): 453–460.









